8 Signs You May Have Insulin Resistance
 By: by Amino Science
By: by Amino Science

According to the Centers for Disease Control and Prevention (CDC), a full one third of adults in the United States have either prediabetes or diabetes. And the vast majority of these cases can be directly linked to a condition called insulin resistance. However, it’s possible to reverse insulin resistance and stop the downward spiral into diabetes. So in this article, we’re going to discuss what causes insulin resistance, eight signs you may have it, and what you can do to turn resistance back into sensitivity.
What Is Insulin Resistance?
Every time you eat or drink something, levels of blood sugar in your body are affected. When everything is functioning normally, beta cells in the pancreas release the hormone insulin in response to rising blood sugar levels. This release of insulin, in turn, helps glucose enter the body’s cells, where it serves as the main source of energy. This process also ensures that blood glucose levels are kept tightly controlled.
However, chronically high concentrations of blood sugar can cause the body to become less sensitive to insulin. In an attempt to compensate for this, the pancreas increases its release of insulin. As long as the pancreas can keep up with the increased demand for insulin, blood sugar will remain in the normal range.
But over time, a constant demand for more and more insulin can damage the cells of the pancreas. When this happens, the body’s cells aren’t able to absorb the excess glucose and blood sugar levels remain high. And this can lead to prediabetes and, eventually, type 2 diabetes—the most common form of diabetes.
According to the CDC, 15% to 30% of people with prediabetes will go on to develop type 2 diabetes within five years. And if left untreated, type 2 diabetes can lead to serious complications, including cardiovascular disease, stroke, nerve damage, limb loss, blindness, kidney failure, nonalcoholic fatty liver disease, and death.
Yet both type 2 diabetes and prediabetes—and possibly metabolic syndrome as well—can be avoided by addressing insulin resistance.
Risk Factors for Insulin Resistance
Several factors can increase your risk of developing insulin resistance. The most common of these are:
- Family history: People with a family history of insulin resistance are more likely to develop the condition themselves.
- Age: Susceptibility to insulin resistance increases with age.
- Race: Racial and ethnic minorities have a greater chance of developing insulin resistance.
- Weight: Excess weight is associated with the development of insulin resistance.
- Abdominal fat: People with increased fat around the abdomen have a greater chance of developing insulin resistance.
- Physical activity: People who lead sedentary lifestyles have a greater risk of insulin resistance.
- Smoking: People who smoke have a greater chance of developing insulin resistance.
- Sleep: People who are chronically deprived of sleep have a higher risk of developing insulin resistance.
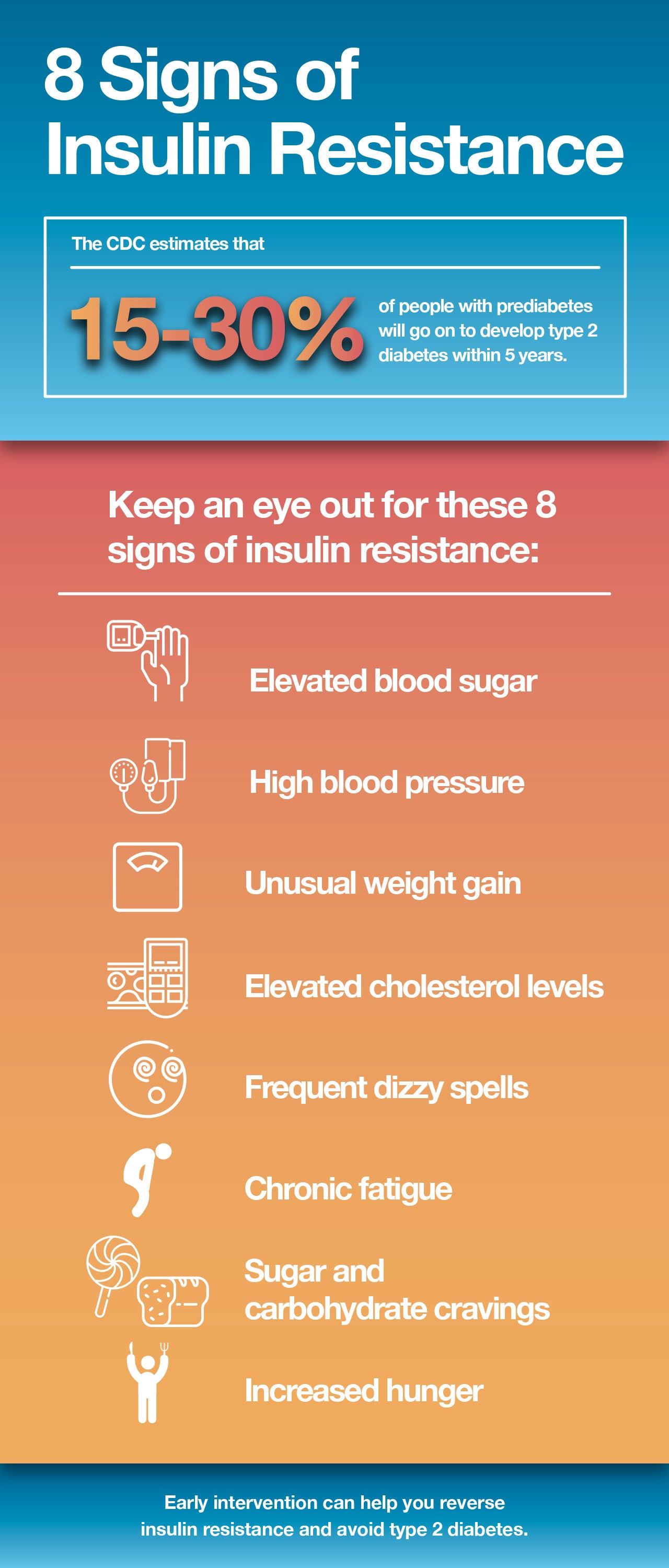
8 Signs of Insulin Resistance
Unless you know what you’re looking for, the signs of insulin resistance can be easy to miss. But by being aware of your risk factors and keeping an eye out for certain signs and triggers, you can begin to see the pattern of insulin resistance and make changes to help reduce your risk of progressing to prediabetes and diabetes.
1. Elevated Blood Sugar
Perhaps the most common method of discovering insulin resistance, prediabetes, and diabetes is measuring fasting blood sugar levels. A fasting blood glucose is taken after not eating for at least 8 hours. But unless you have a blood glucose meter at home, your health care professional will need to perform this test.
Because levels of insulin in the blood may be elevated for years before blood sugar becomes noticeably high, an even more effective test may be the glucose tolerance test, which measures both blood sugar and insulin levels.
2. High Blood Pressure
The relationship between insulin and blood pressure is quite complex, with factors such as low-grade chronic inflammation and oxidative stress thought to play a role. However, magnesium deficiency due to elevated blood glucose may be a consideration as well.
High blood sugar levels lead to increased excretion of magnesium in the urine. But magnesium is required for more than 300 reactions in the body, including regulation of blood sugar and relaxation of blood vessels. Loss of this important mineral as part of insulin resistance can prevent blood vessels from fully relaxing, thus raising blood pressure.
3. Unusual Weight Gain
Insulin resistance is strongly linked to the formation of excess fat cells in the abdominal region. This is actually an evolutionary trait designed to help us survive periods when food may be scarce. However, our modern lifestyles have turned this advantage into a disadvantage, as excess abdominal fat cells lead to impaired insulin signaling, which leads to insulin resistance, which leads to yet more belly fat. A 2012 study postulates that this vicious cycle may be the result of excess fatty acids entering the liver.
4. Elevated Cholesterol Levels
Both type 2 diabetes and insulin resistance are associated with high levels of triglycerides and low levels of high-density lipoprotein (HDL)—the so-called good cholesterol. However, high triglycerides and low HDL are also seen in insulin-resistant individuals with normal blood sugar levels. And the more advanced the insulin resistance, the worse this marker for both diabetes and heart disease becomes.
5. Frequent Dizzy Spells
It may seem counterintuitive, but insulin resistance can also lead to episodes of hypoglycemia, or low blood sugar. When hypoglycemia occurs in the context of insulin resistance, it’s known as reactive hypoglycemia—a response to excess secretion of insulin after a high-carbohydrate meal. Because insulin affects the entire body, both high and low levels can cause dizziness.
When elevated blood glucose is present, dehydration may occur and lead to dizziness. In cases of low blood sugar, however, dizziness can arise as a result of the brain not having enough glucose to function normally.
6. Chronic Fatigue
Chronic fatigue is a classic symptom of insulin resistance. Because glucose is the body’s main source of fuel, the difficulty delivering glucose to the cells that defines insulin resistance means the body doesn’t have enough energy to function properly. Likewise, episodes of reactive hypoglycemia can limit the availability of glucose, which can also lead to fatigue.
7. Sugar and Carbohydrate Cravings
If the only foods that pique your interest are loaded with sugar and carbohydrates, you’re probably experiencing insulin resistance. When cells have trouble absorbing glucose and the body becomes insulin resistant, cravings for foods with a high glycemic index—the measure of the effect on blood sugar levels—increase.
This may seem contradictory, but when the cells can’t get glucose in, they basically respond as if they’re starving, which triggers the body to demand more of the very foods that led to the problem in the first place.
8. Increased Hunger
Just like cravings for sugar and carbohydrates, the inability to get glucose into the body’s cells leads to constant feelings of hunger. The medical term for this is polyphagia, and it’s one of the classic signs of diabetes.
If you see yourself in any of these eight signs, know that you can reverse the process and get back to healthy insulin levels. And simple lifestyle changes are generally all that’s needed.
How to Reverse Insulin Resistance
If you’re overweight, the most effective way to reverse insulin resistance is to lose weight. In fact, weight loss of just 7%, combined with moderate physical activity, can reduce the risk of progressing to type 2 diabetes by 58%.
Likewise, dietary changes that focus on reducing simple sugars and starches and incorporating more whole grains, fruits, vegetables, lean protein, and healthy fats can stabilize your blood sugar levels. Foods that can help reverse insulin resistance include:
| Buckwheat | Poultry |
| Fish | Eggs |
| Apples | Broccoli |
| Sweet potatoes | Brown rice |
| Quinoa | Nuts |
| Olive oil | Spices |
We’re not going to lie to you. In the beginning, this can be a difficult transition, as your cells will be screaming for sugar. But as your blood glucose begins to level out, your cells will again be able to utilize glucose properly, and the cravings and constant hunger will stop.
In addition, getting plenty of sleep and exercising regularly have both been shown to be absolutely essential for improving insulin sensitivity. In fact, a study from 2010 found that it takes only one night without good sleep to cause symptoms of insulin resistance. And a 2014 study demonstrated that weight loss of 10% through diet and exercise improved insulin sensitivity by 80%, while the same amount of weight loss using diet alone was associated with an improvement of 38%.
Branched-Chain Amino Acids and Insulin Resistance
Finally, we’d like to discuss the controversy surrounding insulin resistance and branched-chain amino acids (BCAAs)—leucine, isoleucine, and valine. BCAAs are essential amino acids, which means they can’t be produced in the body and must be supplied via the diet.
It’s a recognized fact that insulin resistance is associated with elevated blood concentrations of BCAAs. And some have interpreted this to mean that BCAAs contribute to the development of insulin resistance. However, multiple studies have shown that taking amino acid supplements that contain BCAAs actually reduces the occurrence of insulin resistance.
This has been demonstrated in cases in which leucine has been used alone or with other essential amino acids or in the context of a balanced mixture of essential amino acids, as evidenced by a 2015 study published in the Journal of Endocrinology, Diabetes, and Obesity and a 2008 study published in the American Journal of Cardiology.
In looking at this evidence, it appears that elevated blood levels of BCAAs are a symptom of insulin resistance and not a cause. Furthermore, supplementation with a balanced mixture of essential amino acids that contains all the BCAAs may be effective in helping reverse insulin resistance.
Hyperlipidemia (high LDL cholesterol and triglycerides) and insulin resistance increase the risk of developing heart disease and metabolic syndrome. Studies confirm that supplementing with essential amino acids can help LDL cholesterol levels and improve blood sugar levels.
If you’re experiencing any signs or symptoms of insulin resistance, we urge you to speak with your health care provider. They can guide you to the treatment plan and lifestyle changes that can help you reverse insulin resistance and avoid type 2 diabetes.

Up to 25% off Amino
Shop NowTAGS: conditions
Join the Community
Comments (0)
Most Craveable Recipes




 833-264-6620
833-264-6620



















