Coronavirus and Heart Health: Why Even the Young and Healthy Are at Risk
 By: by Amino Science
By: by Amino Science

Two studies linking COVID-19 to heart complications were released just last month (July 2020), right on the heels of Boston Red Sox pitcher Eduardo Rodriguez’s announcement that he’d be sitting out the season due to coronavirus-related heart inflammation. As scientists scramble to understand the virus and its associated complications, as well as set standards for treatment and prevention, a troubling trend is emerging: a notable connection between coronavirus and heart health. Emerging evidence suggests that no one, not even the young and healthy, is immune to the virus’s potentially damaging effects on the heart.
Scientific Studies Examining Coronavirus and Heart Health
A number of lingering symptoms have been linked to the coronavirus disease:
- Brain fog
- Shortness of breath
- Extreme fatigue
- Achy joints
- Loss of smell
- Lung damage
- Chest pain
- Rapid heart rate
- Unexplained swelling
And it appears that the following heart-related symptoms join this list:
- Heart attack
- Heart inflammation
- Heart failure
- Irregular heartbeat
- Blood clots in veins
These are the cardiovascular consequences of COVID-19 according to a report published April 2020 in the American Journal of Emergency Medicine as evidenced by 45 studies, including case studies, systematic reviews and meta-analyses, and retrospective and prospective studies (1).
A study published a month earlier in JAMA Cardiology determined that 1 out of every 5 COVID-19 patients exhibit signs of heart damage regardless of whether they had accompanying respiratory distress. Some of these patients had underlying heart conditions, while others had a prior clean bill of health only to go on to develop complications such as blood clots, blood vessel injuries, arrhythmias, strokes, and heart attack (2).
Blood clots, particularly in the lungs and legs, took center stage early on as a coronavirus complication in otherwise healthy individuals. First came the anecdotal accounts, followed by a report from Mount Sinai doctors that was published in the New England Journal of Medicine (3). Doctors on the frontlines reported strokes in 5 COVID-19 patients in their 30s and 40s.
These reports were followed by similar accounts all over the world—88 patients in China, 6 patients in England, and 3 patients in France all suffered from strokes (4,5,6). In response to the connection between COVID-19 and blood clots, doctors began treating certain patients with blood thinners and found that doing so could decrease the likelihood of death in patients on ventilators.
The two most recent studies published in JAMA Cardiology paint a similarly bleak picture. Researchers from the University of Frankfurt compared the cardiac MRIs of patients who had recovered from COVID-19 to people who had not contracted the virus (7). Those who’d been infected with the coronavirus were much more likely to show heart injury.
- 78 patients had structural changes to the heart muscle
- 76 showed evidence of heart damage mimicking the aftermath of a heart attack
- 60 had chronic cardiac inflammation
Lead researcher and cardiologist Valentina Puntmann stated, “The fact that 78% of ‘recovered’ [patients] had evidence of ongoing heart involvement means that the heart is involved in a majority of patients, even if Covid-19 illness does not scream out with the classical heart symptoms, such as anginal chest pain.”
It should be noted that of the 100 coronavirus patients studied, two-thirds of them had mild symptoms and recovered at home. The lasting implications of the virus may prove to be far more distressing than the initial symptoms.
The second study examined autopsy results of 39 coronavirus victims (average age of 85) and discovered high levels of the virus in the hearts of 24 of them (8).
The takeaway from each of these studies is clear: COVID-19 could lead to any manner of heart complications, including heart failure.
What’s Happening Behind the Scenes?
There is much to learn about the coronavirus and cardiac injury, but scientists have pinpointed three ways the virus compromises heart health:
- Inciting systemic inflammation
- Directly infecting the cardiovascular system
- Exacerbating preexisting conditions
The virus responsible for COVID, called SARS-CoV-2, is known for going after the lungs, but it can also stimulate the body’s immune response to such a degree that it triggers a cytokine storm of ongoing inflammation throughout, including inflammation of the heart, a condition called myocarditis. This diminishes the heart’s ability to pump blood and transmit electrical signals, which in turn can lead to abnormal heart rhythms and heart disease.
We know SARS-CoV-2 can also go after the heart directly by attaching to a receptor called angiotensin converting enzyme 2 (ACE2), which resides mostly in the lungs but also in the heart and blood vessels. Once attached to ACE2, COVID can lead to cell dysfunction and death.
While no one is immune to the effects of COVID on heart health, those with preexisting health conditions are especially susceptible to heart problems. And heart patients are the most at risk according to study of over 72,000 coronavirus cases (9).
| CONDITION | FATALITY RATE |
| Heart Disease | 10.5% |
| Diabetes | 7.3% |
| Chronic Respiratory Disease | 6.3% |
| Cancer | 5.6% |
Cardiovascular disease already places a strain on your heart and blood vessel function, and COVID further compromises blood flow to the heart.
Research has also shown that treatment medications such as nonsteroidal anti-inflammatory drugs (NSAIDS), glucocorticoides, and antiviral drugs can increase risk of death in people with underlying conditions. NSAIDS can elevate blood pressure, glucocorticoides can lower inflammation but raise blood sugar levels, which can have dire consequences in cardiovascular or diabetes patients, and antivirals can lead to arrhythmias and a wearing away of heart muscle, which can impair heart recovery over the long term. Studies indicate that the controversial antivirals hydroxychloroquine and remdesivir may lead to heart damage and make preexisting conditions worse in some COVID patients (1).
If you are currently on medications for preexisting conditions, such as ACE inhibitors and angiotensin receptor blockers, and you are diagnosed with the coronavirus, it is important to follow the counsel of your doctor, who will have the most up-to-date information on how these medications interact with treatment.
Staying Safe
COVID research is ever evolving, and we do not know if heart complications from COVID will eventually resolve on their own or remain chronic. We do know that this viral infection can impact both healthy hearts and hearts already battling coronary artery disease, congenital birth defects, and other heart issues. Likewise older individuals with high blood pressure, stroke survivors, diabetics, and people with lung disease or immune disorders are at higher risk of more severe symptoms.
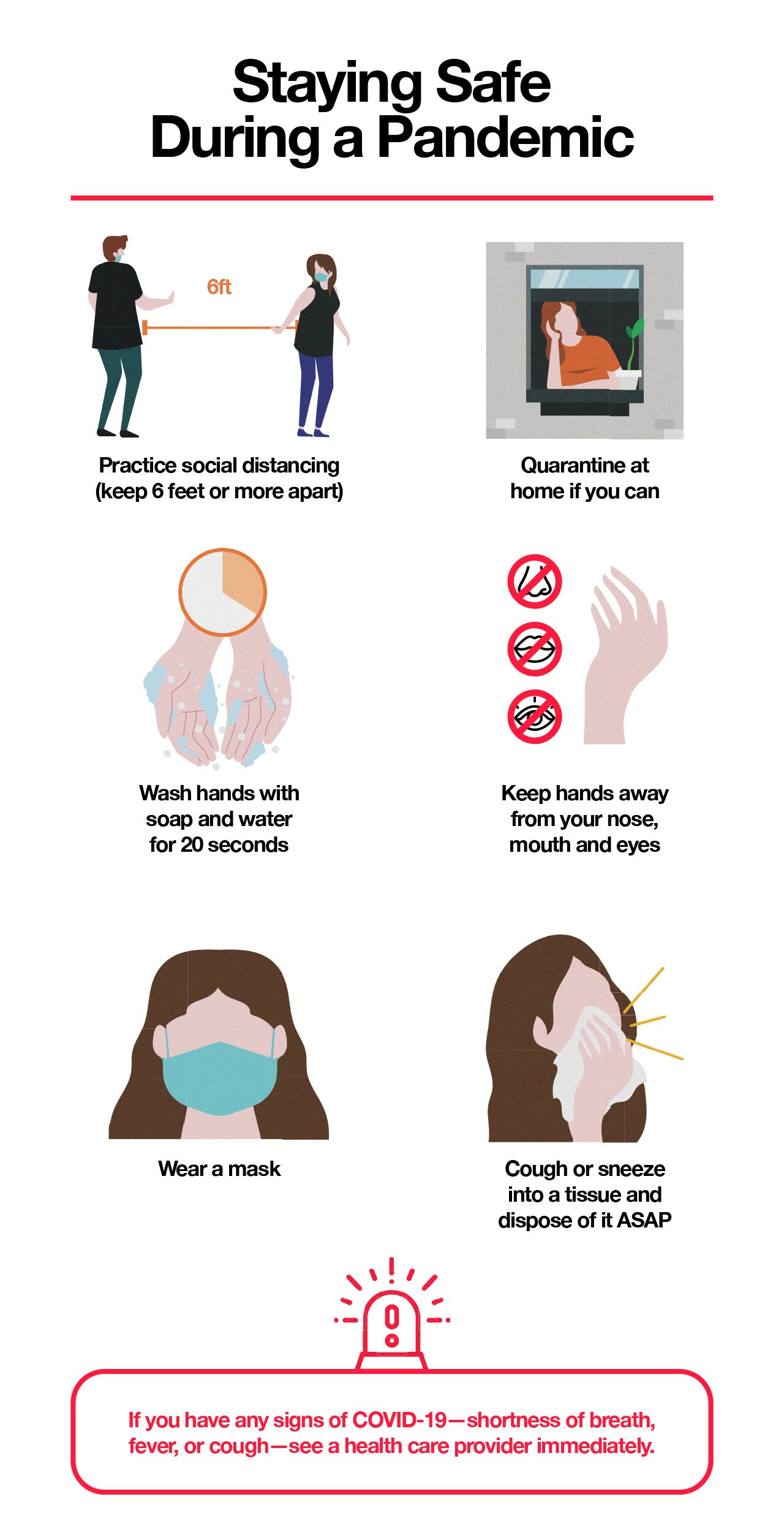
We recommend following the guidance of the CDC and American Heart Association during this pandemic:
- Practice social distancing (keep 6 feet or more apart)
- Quarantine at home if you can
- Wash hands with soap and water for 20 seconds
- Keep hands away from your nose, mouth, and eyes
- Wear a mask
- Cough or sneeze into a tissue and dispose of it ASAP
If you have any signs of COVID-19—shortness of breath, fever, or cough—see a health care provider immediately. And if you are experiencing the signs of a stroke or heart attack, call 911.
In the meantime, keep your heart and health in top condition with the support of essential amino acids.

Up to 25% off Amino
Shop NowTAGS: conditions
Join the Community
Comments (0)
Most Craveable Recipes





 833-264-6620
833-264-6620



















