Diverticulosis and Diverticulitis Explained
 By: by Amino Science
By: by Amino Science

Diverticulosis, also called diverticular disease of the colon, is common in the United States. In fact, according to the American Society for Gastrointestinal Endoscopy, diverticulosis affects half of everyone over age 60 and nearly everyone by age 80. The good news is that even though diverticulosis may sound scary, most people don’t even know they have it. But sometimes, diverticulosis can lead to another condition called diverticulitis. According to Harvard Medical School, about 15-20% of people with diverticulosis go on to develop diverticulitis. So what is the difference? How serious is diverticulitis and is there a way to prevent it?
Keep reading for a breakdown of diverticulosis, diverticulitis, causes, symptoms, and treatments.
What Is Diverticulosis?
Diverticulosis is a condition in which diverticula, or pouches, have formed in the lining of the digestive tract. The outer layers of the digestive tract wall can have weak spots. The pouches form when inner layers of the digestive tract wall push through these weak spots in the outer layers. Diverticula usually form in the colon and can be isolated to specific spots or occur throughout the colon. While the diverticula often cause no problems, they can sometimes become inflamed or infected and cause bleeding or bowel obstruction. When the diverticula become infected or inflamed, it is a condition known as diverticulitis.
What Causes Diverticulosis?
Diverticulosis is less common in certain parts of the world, particularly regions where diets tend to be high in fiber, grains, fruits, and vegetables. This leads physicians to believe that a low-fiber diet may be a contributing factor in the development of diverticulosis. Low-fiber diets often lead to constipation, which in turn leads to straining and pressure in the digestive tract. If pressure and straining persist for long periods of time, diverticulosis may develop.
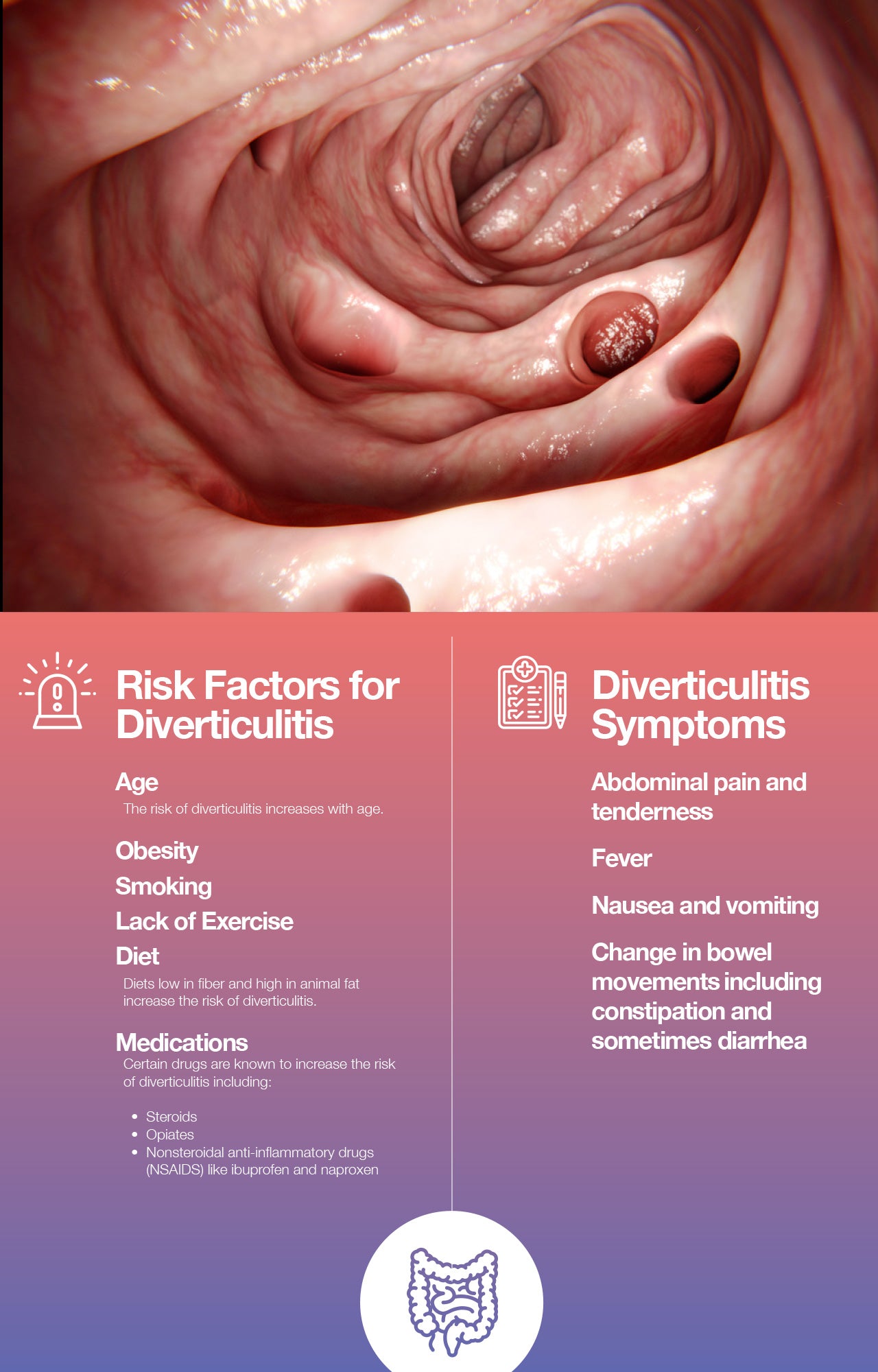
There are a few actions one can take to decrease the risk of diverticulosis developing into diverticulitis. According to the Mayo Clinic, certain lifestyle choices play a role in the development of diverticulitis.
Symptoms of Diverticulosis and Diverticulitis
Diverticulosis often causes no symptoms, and many people are unaware that they even have the condition. However, diverticulosis can sometimes cause difficulty passing stool, which may result in symptoms like constipation, bloating, or cramps. Most people only experience symptoms if the diverticula become inflamed or infected, leading to diverticulitis.
Diagnosing Diverticulosis and Diverticulitis
Since most people experience no symptoms of diverticulosis, the condition is often found during routine screenings and checkups for other conditions. For example, it is often discovered during a routine colonoscopy screening for colon polyps or colon cancer.
If a physician suspects diverticulitis, he or she will likely order a series of tests to rule out other possible conditions that may present with similar symptoms. Common tests ordered include:
- Blood and urine tests to check for infection
- Pregnancy tests for women
- Liver function tests
- Stool test
Once other possible causes of the symptoms have been ruled out, the physician will likely order a CT scan. A CT scan can show the presence of infected diverticula and confirm a diagnosis of diverticulitis.
Diverticulitis Treatment
Diverticulosis usually does not come with symptoms, so treatment typically isn’t necessary. However, if diverticulitis develops, then the patient does need treatment. Treatments vary from patient to patient and case to case depending upon the severity of the diverticulitis. Common treatments include:
- Antibiotics
- A liquid diet while the digestive tract heals
- Over-the-counter pain relievers
These treatments are most often used at home by patients. Severe cases of diverticulitis may require hospitalization, IV antibiotics, and possible surgery. Surgery is sometimes necessary if an abscess, fistula, or bowel obstruction has formed.
Diverticulosis Diet
There are certain dietary choices that one can make to help prevent or treat a case of diverticulitis.
To help prevent diverticulitis:
- Eat more fiber. Try incorporating more high-fiber foods into a regular diet routine. High-fiber foods include fruits, vegetables, and grains. An increase in fiber will not get rid of existing diverticula, but it may help prevent new ones from forming.
- Drink more water. Fiber is only beneficial if enough liquids are being taken in. If not, a high-fiber diet can lead to constipation, which can in turn lead to diverticulitis.
The Mayo Clinic suggests the following diet to allow the digestive tract to heal from diverticulitis:
- Clear liquids:
- Broth
- Apple juice
- Ice chips
- Popsicles
- Water
- Tea or coffee
- Low-fiber foods:
- Eggs
- Poultry
- Fish
- Fruit juice
- Low-fiber cereals
- Milk, yogurt, and cheese
- White rice, pasta, and noodles
- Canned or cooked vegetables without the skin
- Canned or cooked fruits without the skin or seeds
While there is no evidence yet that specific supplements help prevent or cure diverticulitis, the Penn State Hershey Medical Center does cite the amino acid glutamine as providing intestinal health benefits. Amino acids are essential for maintaining a healthy body. They help the body make protein and chemicals needed for proper and healthy functioning.
Amino Acids
Even though the amino acid glutamine may benefit intestinal health, it's best to take a balanced mixture of all essential amino acids to make sure that the blood concentration of amino acids is optimal. Additionally, glutamine may not be a good choice for everyone. The Penn State Hershey Medical Center states that those with diabetes, seizures, liver disease, or a history of mania or manic episodes should not take glutamine. Anyone considering adding supplements of any kind should speak with his or her physician first to make sure it is a good idea.

Up to 25% off Amino
Shop NowTAGS: conditions
Join the Community
Comments (0)
Most Craveable Recipes




 833-264-6620
833-264-6620



















