Fatty Liver Disease: Improving Liver Health with Amino Acids and Other Natural Strategies
 By: by Amino Science
By: by Amino Science

The liver is the body’s largest internal organ. And while it’s responsible for carrying out an estimated 500 different tasks—including acting as the body’s primary site for nutrient processing and lipid, carbohydrate, and amino acid distribution—it’s perhaps best known for its role in filtering the body’s blood supply. Yet for all the impressive things the liver does to keep us alive and healthy, certain conditions can compromise its ability to function. By far, the most common condition to negatively impact the liver is fatty liver disease, which affects up to a quarter of all adults in the United States.
In this article, we’re going to discuss what fatty liver disease is, the signs and symptoms to watch out for, and the role amino acids as well as other natural strategies and lifestyle changes may play in preventing and even reversing this potentially serious medical condition.
What Is Fatty Liver Disease?
A normal, healthy liver converts excess carbohydrates and proteins from the foods we eat into fatty acids and triglycerides. These substances are then used by the body as a source of energy or sent out into the blood to be stored as fat in the peripheral adipose tissue.
Ordinarily, only a small amount of triglycerides are stored in the liver. However, various conditions—including alcoholism, obesity, insulin resistance, type 2 diabetes, high blood pressure, high cholesterol, and hepatitis C—can reduce the liver’s ability to metabolize excess fat, which may then build up in the liver.
And if the amount of fat in the liver increases to more than 5% to 10% of total liver volume, fatty liver disease, or hepatic steatosis, becomes an issue.
Types of Fatty Liver Disease
Many people think fatty liver disease refers to one specific condition, but that’s actually not the case. In fact, there are two main types of fatty liver disease.
Alcoholic Fatty Liver Disease
This first stage of alcoholic liver disease, which is also known as alcoholic steatohepatitis, is the result of years of heavy alcohol use. While the liver can handle moderate alcohol intake, excessive drinking impairs its ability to break down fatty acids, which can lead to high triglyceride levels, liver inflammation (alcoholic hepatitis), and the formation of scar tissue (cirrhosis).
If caught in the early stages, abstaining from alcohol for as little as 2 weeks can help the liver clear out the excess fat and resume normal function. However, over time, the liver damage that results from constant heavy drinking can lead to chronic liver disease, with loss of liver cells, irreversible scarring of the liver, and increased risk of liver cancer, liver failure, and need for liver transplant.
Nonalcoholic Fatty Liver Disease
NAFLD affects an estimated 80 to 100 million Americans, many of whom don’t even know they have the condition. While NAFLD can manifest as simple fatty liver, with little or no inflammation or damage to liver cells, it can also progress to nonalcoholic steatohepatitis (NASH)—a condition in which inflammation and liver cell damage are both present. Like alcoholic liver disease, NASH can eventually lead to severe liver inflammation and scar tissue and increase the risk of liver cancer, failure, and transplant.
Symptoms of Fatty Liver Disease
Unfortunately, it can be hard to know if you have fatty liver disease because the early stages often present with no symptoms. Therefore, most people discover they have the condition when blood tests or imaging tests performed for other reasons indicate a liver problem.
In addition, even though fatty liver disease may result in elevations in liver enzymes, many people with the condition have perfectly normal enzyme levels. Even people whose fatty liver disease has progressed to cirrhosis may continue to have normal liver enzymes.
While this certainly doesn’t help with diagnosis, it is a testament to the liver’s amazing regenerative powers, which enable it to continue to function when as much as 75% of it has been damaged.
If liver enzyme levels are elevated, a definitive diagnosis will require a liver biopsy to determine whether the cause of the elevation is indeed fatty liver disease or something else, such as a viral infection.
However, as fatty liver disease progresses and the liver’s ability to function becomes more and more compromised, signs and symptoms will become increasingly more apparent and may include:
- Liver enlargement
- Loss of appetite
- Weight loss
- Fatigue
- Itching
- Upper right abdominal pain
- Ascites (abdominal fluid)
- Jaundice (yellowing of the skin)
- Visibly enlarged blood vessels
Treatment of Fatty Liver Disease
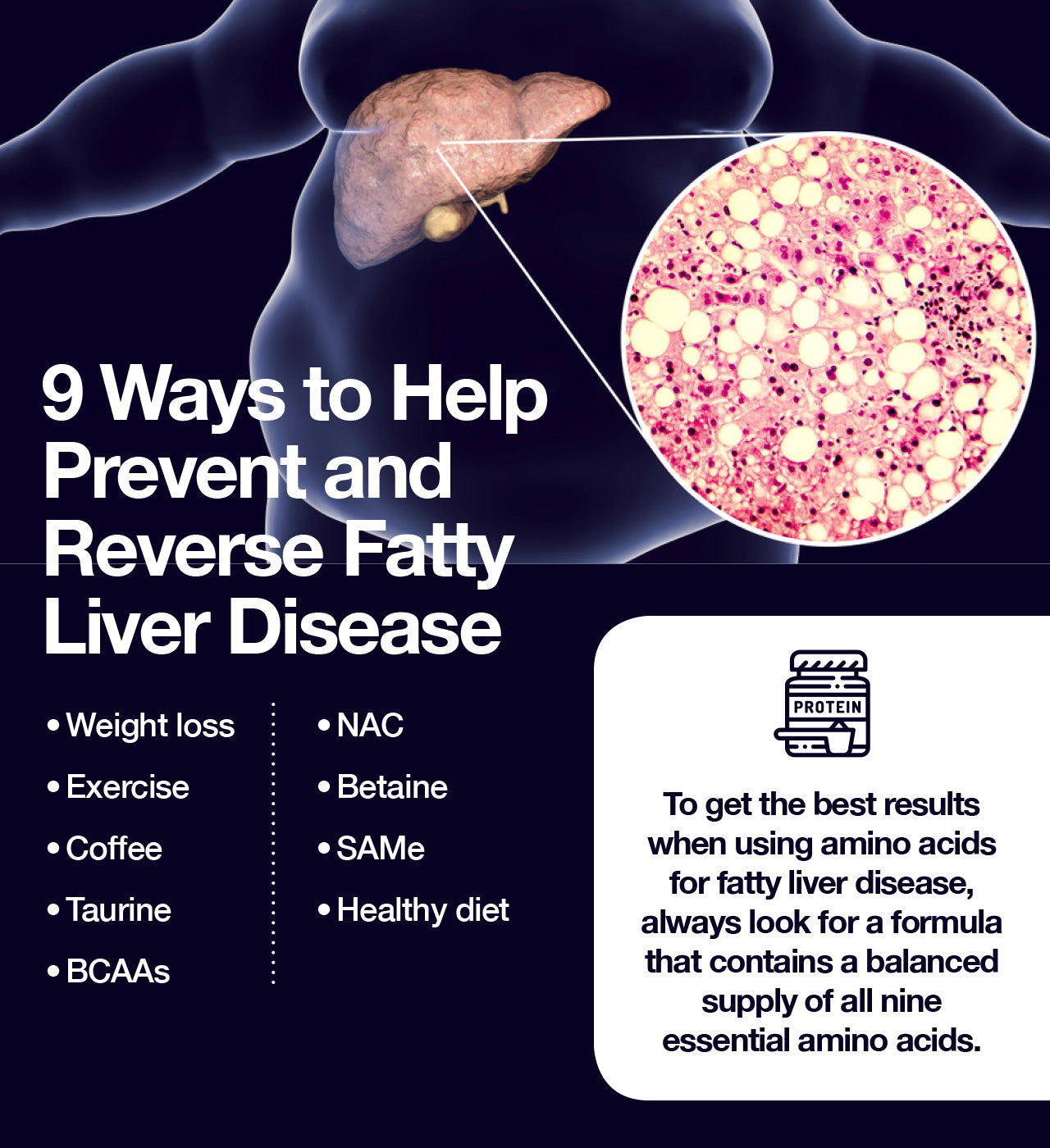
Although no medications are currently approved for the treatment of fatty liver disease, a number of natural approaches have been found to be helpful in both treating and reversing the damage caused by excess fat in the liver.
Beyond decreasing alcohol intake, experts agree that the most effective way to treat fatty liver disease is by maintaining a healthy body weight.
In fact, a 2016 study found that weight loss of just 3% to 6% results in a reduction in liver fat of 35% to 40%. And another study from the same year demonstrated that weight loss of 7% to 10% not only is associated with reduced liver fat but can also lead to complete remission of NASH and a reduction in scar tissue.
Like weight loss, physical activity is also recommended for treatment of fatty liver disease.
A 2018 review of 30 randomized controlled trials found overwhelming evidence to support the use of exercise in the treatment of fatty liver disease. The study’s authors found that a variety of both aerobic and resistance training exercises can reduce excess liver fat by improving insulin resistance, fatty acid metabolism, and function of mitochondria (the energy centers of the cells) and by decreasing levels of inflammation.
While weight loss and exercise are two of the most important components of an effective fatty liver treatment plan, they’re not the only factors that have been shown to have a positive effect on liver health.
Coffee
Coffee was once blamed for everything from stunted growth to heart disease, but more and more scientific research is suggesting that the bitter brew is actually a complex substance with a wide range of amazing health benefits—benefits that may have a positive impact on liver function as well.
For example, a 2017 study found that daily coffee consumption can help protect against liver cancer as well as “chronic liver disease secondary to alcohol, viral hepatitis, and fatty infiltration.” And a 2015 study found that people who consume 3 or more cups a day of either regular or decaffeinated coffee have lower liver enzyme levels.
A 2016 study also found that coffee is particularly beneficial for people with liver disease, and consumption of 2 or more cups a day can protect against both liver cancer and the fibrosis (scarring) seen in cirrhosis. Moreover, the study’s researchers emphasized that coffee protects the liver against all forms of disease, though it appears to be most protective against alcoholic liver disease.
Amino Acids
Regular supplementation with essential amino acids is a proven natural and effective treatment for fatty liver.
For example, a 2018 study found that the sulfur-containing amino acid taurine was able to suppress oxidative stress and fatty acid accumulation in the livers of mice fed high-fat diets, leading researchers to conclude that supplementation with taurine may help reduce the risks associated with NAFLD.
Another rodent study, this one from 2012, found that supplementation with the branched-chain amino acids (BCAAs) leucine, isoleucine, and valine was able to reduce scar tissue and liver cell death and delay the progression of chronic liver disease in rats with induced liver disease.
Cysteine—which is available in supplement form as N-acetylcysteine (NAC)—is another sulfur-containing amino acid with potent antioxidant properties that protect cells from oxidative stress.
A 2010 clinical trial involving 30 individuals with NAFLD demonstrated that supplementation with NAC resulted in a significant decrease in liver enzyme levels as well as spleen size (a symptom of liver disease) compared with vitamin C, leading researchers to conclude that NAC can improve liver function in patients with NAFLD.
Several small studies have also found that S-adenosylmethionine (SAMe)—which is composed of the amino acid methionine bound to a molecule of adenosine triphosphate (ATP)—helps protect liver cells and prevent progression of fatty liver disease.
One of these studies demonstrated that supplementation with the choline metabolite betaine naturally raises levels of SAMe in the body and reduces scarring, liver enzyme levels, and degree of fatty infiltration, leading to significant improvement in patients suffering from NASH.
Because amino acids contribute to overall health by working in concert with one another to support the numerous biochemical processes of the body, the positive effects on fatty liver disease seen with these building blocks of protein may be even further enhanced by using them as part of a balanced formula containing all nine essential amino acids.
Diet
Diets high in trans fats, simple sugars, red meat, salt, and fried and processed foods are associated with a number of health conditions, from obesity to high blood pressure and cholesterol to prediabetes and type 2 diabetes to—you guessed it—fatty liver disease.
However, healthy diets rich in fruits and vegetables, whole grains, lean meats, and good fats can help prevent and treat all these conditions.
If you’re currently suffering from or at risk of fatty liver disease, some foods to get you back on the road to health include:
- Fish
- Tofu
- Avocados
- Olive oil
- Broccoli
- Nuts
- Seeds
And if you’re already dealing with insulin resistance, metabolic syndrome, prediabetes, or type 2 diabetes, it’s extremely important that you get your blood sugar under control, as fatty liver disease occurs in at least half of all individuals with diabetes.
Finally, if you have risk factors, don’t hesitate to speak with your health care provider about lifestyle changes you can implement to decrease your risk of developing fatty liver disease. The sooner you take steps to lower your risk, the better your chances of avoiding this potentially life-threatening condition altogether.

Up to 25% off Amino
Shop NowTAGS: conditions liver natural cures
Join the Community
Comments (0)
Most Craveable Recipes




 833-264-6620
833-264-6620



















