Necrotizing Fasciitis: Flesh-Eating Disease Causes, Symptoms, Treatment
 By: by Amino Science
By: by Amino Science
Necrotizing fasciitis, more popularly known as flesh-eating disease, is a rare but potentially fatal infection that affects approximately 200,000 people worldwide each year. While many different bacteria, and even fungi, are known to cause necrotizing fasciitis, the Centers for Disease Control and Prevention (CDC) tracks what’s generally considered to be the most common cause—group A Streptococcus, the same bacteria that cause strep throat. According to the agency’s estimates, approximately 700 to 1,200 cases of necrotizing fasciitis occur each year in the United States as a result of group A Streptococcus.
Although the number of cases may seem relatively small, it’s important not to underestimate this life-threatening illness, so read on to discover what causes necrotizing fasciitis and how to recognize the symptoms and seek treatment.
Causes of Necrotizing Fasciitis
Necrotizing fasciitis is an infection of the fascia—a type of connective tissue that surrounds muscles and other internal organs. The result of what’s commonly known as flesh-eating bacteria or, in rare cases, fungi, necrotizing fasciitis spreads rapidly along the fascial plane as the invading organisms multiply and release toxins and enzymes that lead to thrombosis, or clotting, of blood vessels. This clotting of the vessels, in turn, results in decreased blood supply to the surrounding subcutaneous tissues and subsequent necrosis, or tissue death.
The bacteria and fungi that cause necrotizing fasciitis usually enter the body through breaks in the skin, though blunt injuries, such as bruises, have also been known to cause the disease. Some of the most common triggers for necrotizing fasciitis include:
- Puncture and surgical wounds
- Insect bites
- Scrapes
- Cuts
- Burns
In addition, some cases in Asia have been linked to “consumption of raw or undercooked seafood or injury by fish fins.” However, in these instances, various types of marine bacteria (Vibrio spp, Aeromonas spp, Shewanella spp) were usually involved.
The majority of cases of necrotizing fasciitis are caused by a combination of aerobic and anaerobic bacteria. While aerobic bacteria require oxygen to proliferate, anaerobic bacteria multiply in low-oxygen environments and produce gas. This gas accumulates within subcutaneous tissues and can cause gas gangrene—a highly lethal condition that can quickly lead to death.
The most common types of bacteria associated with necrotizing fasciitis are:
- Gram-positive cocci (Staphylococcus aureus, Streptococcus pyogenes, and enterococci)
- Gram-negative rods (Escherichia coli and Pseudomonas aeruginosa)
- Anaerobes (Bacteroides and Clostridium species)
Necrotizing fasciitis can occur anywhere on the body, but the most common sites of infection are the extremities and perineum. A rare type of necrotizing fasciitis called Fournier gangrene, which affects the scrotum, penis, or perineum, is especially virulent and spreads even more rapidly than other forms of necrotizing soft tissue infections.
Symptoms of Necrotizing Fasciitis
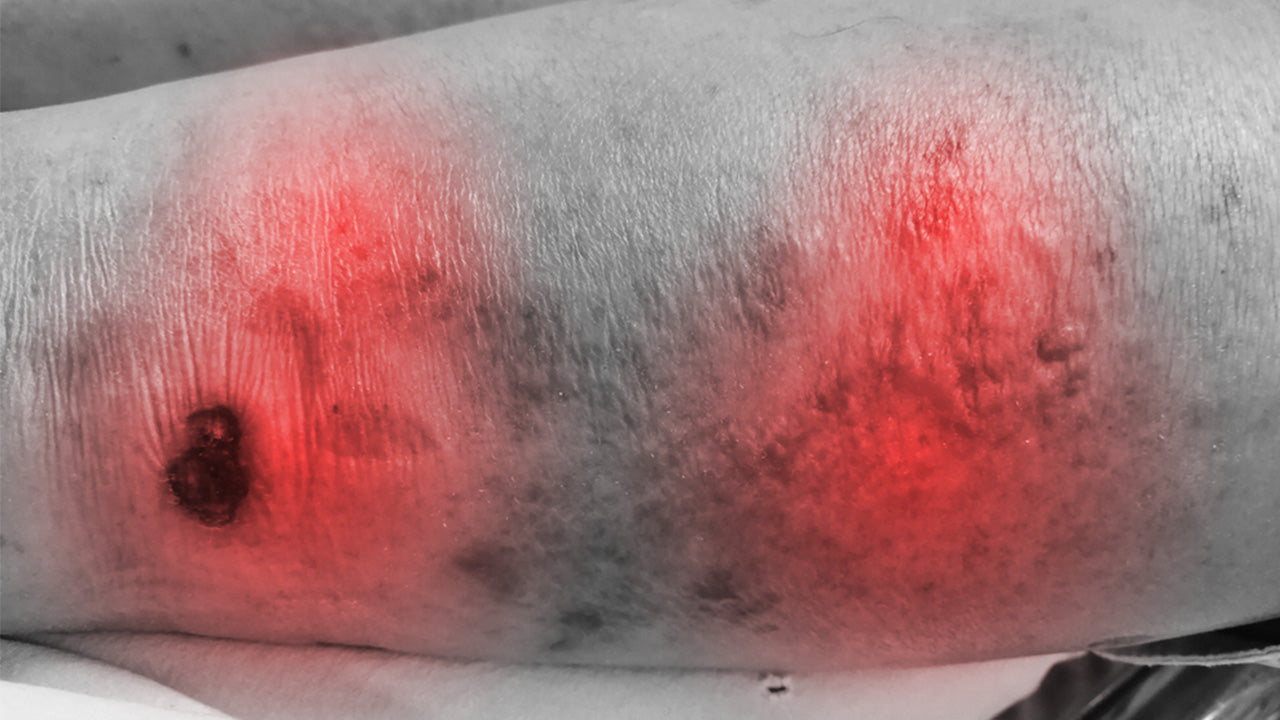
Unfortunately, the early stages of necrotizing fasciitis are hard to distinguish from more benign types of skin infections. The initial symptoms may resemble those of cellulitis—a bacterial infection that causes redness and swelling of the skin, along with warmth, fever, and pain. However, unlike cellulitis, the severe pain felt with necrotizing fasciitis is far greater than what would normally be expected based on the appearance of the infection.
After the initial stages, symptoms of necrotizing fasciitis become more serious and may include:
- Crackling sensation under the skin due to the presence of gas
- Skin discoloration
- Ulcers
- Blisters
- Black scabs
- Draining pus
Complications of Necrotizing Fasciitis
If necrotizing fasciitis isn’t diagnosed and treated in its early stages, the infection can spread to the bloodstream and cause sepsis and septic shock—a severe form of sepsis in which blood pressure drops and organ failure occurs due to lack of oxygen.
Alarmingly, approximately 25% to 33% of people diagnosed with necrotizing fasciitis will die of the disease—a mortality rate that’s the direct result of the difficulty identifying the condition in its early stages, coupled with its rapid progression. And even those who survive may be left with amputations or severe scarring from extensive surgical removal of tissue.
Risk Factors for Necrotizing Fasciitis
Although anyone who’s sustained some type of injury can develop necrotizing fasciitis, some groups are more susceptible to the disease than others. The main risk factors associated with the illness include:
- Peripheral vascular disease
- Immune compromise
- Intravenous drug use
- Age greater than 50
- Diabetes mellitus
- Hypertension
- Alcoholism
- Obesity
A number of studies have found that people with diabetes may be at especially high risk of both developing and succumbing to the disease, with one study showing that over 70% of people diagnosed with necrotizing fasciitis had diabetes as well.

Treatment of Necrotizing Fasciitis
Accurate, early diagnosis of necrotizing fasciitis and immediate, aggressive therapy are essential for a successful outcome, so if your health care provider suspects necrotizing fasciitis, they may begin treatment before a definitive diagnosis is made.
However, an exact diagnosis will depend on obtaining fluid samples or tissue biopsies to isolate the organism or organisms causing the infection. Laboratory studies to look for signs of infection and muscle damage as well as imaging studies—MRI (magnetic resonance imaging), ultrasound, and CT scan (computed tomography)—are also helpful for identifying gas in the subcutaneous tissues and extent of infection.
Because of the seriousness of necrotizing fasciitis, people diagnosed with the illness must be hospitalized—often in the intensive care unit—and treated with intravenous antibiotics. And the sooner this takes place, the better, as antibiotic therapy may not be as effective if treatment begins during the latter stages of the infection.
Other interventions commonly used in the treatment of necrotizing fasciitis include:
- Surgical debridement: In addition to antibiotic therapy, surgical debridement to cut away necrotic tissue is the principal treatment for necrotizing fasciitis. Depending on the extent of the infection, multiple surgical treatments may be necessary, up to and including amputation of the affected limb. However, the earlier debridement is performed, the better a patient’s chances for survival.
- Intravenous immunoglobulin: IVIG therapy involves the administration of antibodies that are used by the immune system to fight foreign invaders. Although IVIG hasn’t yet been approved by the Food and Drug Administration (FDA) for the treatment of necrotizing fasciitis, small clinical trials have shown it has the ability to bind to the toxins released by the staphylococcal and streptococcal bacteria often implicated in the disease.
- Negative pressure wound therapy: NPWT, also called vacuum-assisted wound closure, uses continuously or intermittently applied subatmospheric pressure to promote wound healing.
- Hyperbaric oxygen therapy: HBOT involves exposing the body to 100% oxygen at 3 times the normal air pressure. Like IVIG, HBOT also hasn’t been approved for the treatment of necrotizing fasciitis, but some studies have shown that it can reduce mortality when used as part of an aggressive treatment regimen.
Preventing Necrotizing Fasciitis
Supporting the immune system and practicing good hygiene and wound care are two of the best ways to prevent necrotizing fasciitis. You can help ensure your immune system stays strong by getting plenty of sleep, managing stress, staying hydrated, and eating a diet that limits processed foods and emphasizes fruits, vegetables, whole grains, lean proteins, and healthy fats.
But in our modern age, even the healthiest of diets can sometimes use some extra support, so you might also think about supplementing with a variety of vitamins, minerals, amino acids, and herbs that have been shown to support the immune system and guard against infection. Some top choices include:
- Vitamins C, D, and E
- Elderberry
- Echinacea
- Astragalus
- Arginine
- Olive leaf extract
- Garlic
- Green tea
- Zinc
In addition, essential oils like oregano and tea tree as well as colloidal silver have powerful antimicrobial properties that, when applied directly to a wound, can help stop an infection before it starts.
Although necrotizing fasciitis is a rare infectious disease, you should never take this life-threatening illness for granted. See your health care provider right away if you experience fever, dizziness, or nausea soon after an injury or surgical procedure. It just might save your life.

Up to 25% off Amino
Shop NowTAGS: conditions
Join the Community
Comments (0)
Most Craveable Recipes




 833-264-6620
833-264-6620



















