Pancreatitis Pain: Could You Have Pancreatitis?
 By: by Amino Science
By: by Amino Science

The pain is sharp, behind the stomach, and it sends waves of agony from the upper abdomen out the back. It’s pancreatitis pain, but many people have no idea what it is when an attack comes on. We’re keeping you informed with the essential information you need to know about pancreatitis pain.
What Is the Pancreas?
The pancreas is an essential organ–you can’t live without it. By secreting digestive enzymes into the small intestine, the pancreas helps us digest food so we can absorb nutrients for life, and it plays a critical role in the regulation of blood sugar levels.
When pancreatic enzymes are switched on before they reach the small intestine, they attack the pancreas. And when the pancreas becomes inflamed, the condition is called pancreatitis.
Pancreatitis is a dangerous, life-threatening situation in need of immediate medical attention. Most people do usually seek treatment due to the unbearable pain.
Could you have pancreatitis?
Acute Pancreatitis vs. Chronic Pancreatitis
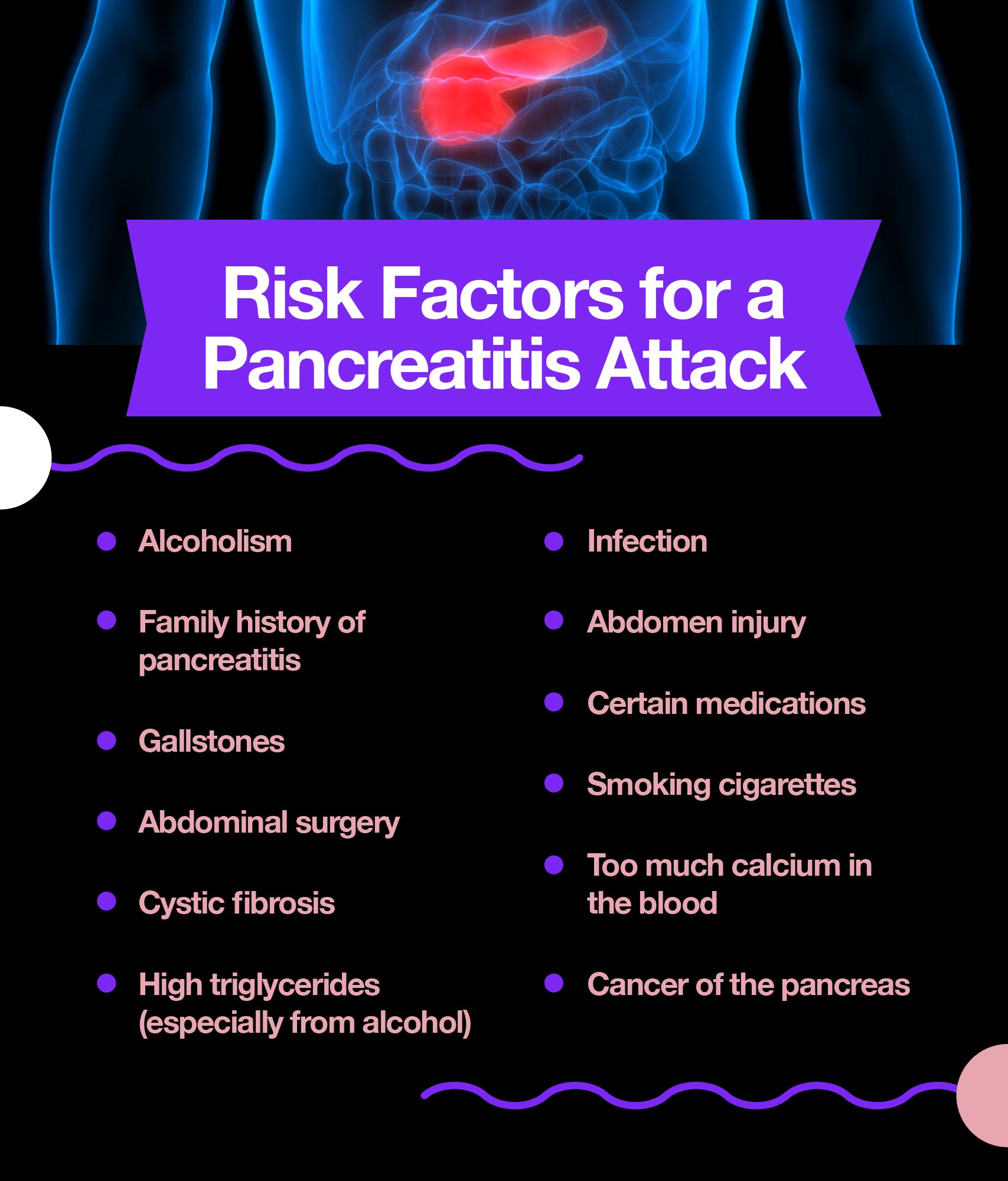
Acute pancreatitis is a sudden attack of inflammation of the pancreas, such as those caused by gallstones and heavy alcohol use. Chronic pancreatitis, on the other hand, comes from damage to the liver over time, due to multiple attacks, chronic alcohol consumption, or conditions such as cystic fibrosis or hereditary pancreatic diseases. Chronic pancreatitis leads to scar tissue, and then the organ stops working correctly. When that happens, a person becomes at risk for diabetes and serious digestive problems, including malnutrition.
The mortality rate of severe acute cases of pancreatitis is high—about 1 in 10, according to The National Pancreas Foundation. However, new research has been leading to new treatments, preventions, and cures. The National Pancreas Foundation also reports that between 16.5% and 25% of patients who experience acute pancreatitis have another attack within the first several years.
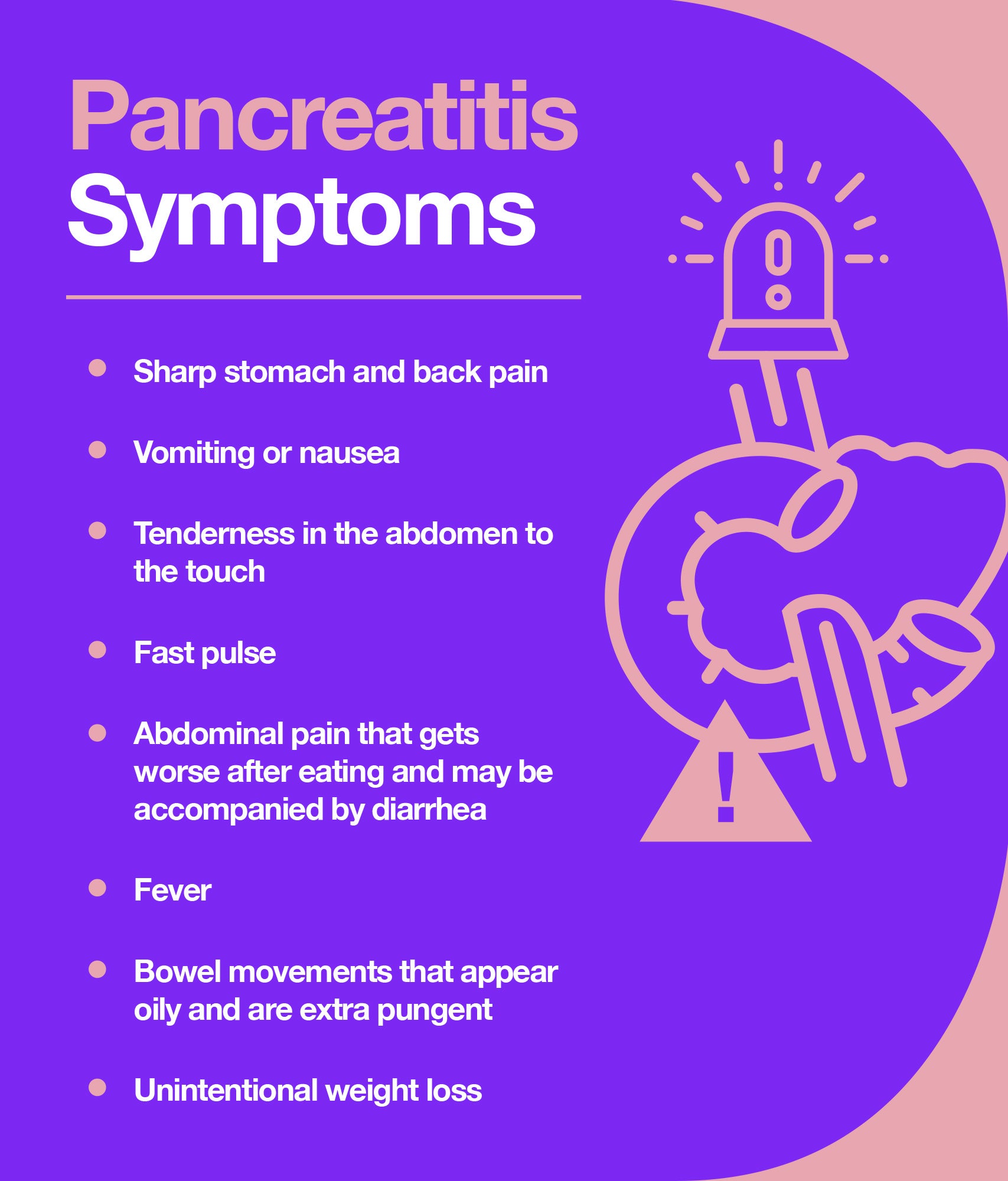
According to the Mayo Clinic, symptoms of acute pancreatitis include:
- Upper abdominal pain
- Abdominal pain that worsens after a meal
- Abdominal pain that extends to your back
- Fever
- Rapid pulse
- Nausea and vomiting
- Tender abdomen
Symptoms of chronic pancreatitis include:
- Upper abdominal pain
- Unexplained weight loss
- Oily, smelly stools
Pancreatitis Complications
Many people with acute pancreatitis develop pancreatitis complications, many of which are life-threatening.
- Infection: During bouts of acute pancreatitis, cysts form in the pockets of the pancreas. The fluid-filled cysts can rupture and cause internal bleeding and infection. In cases of chronic pancreatitis, the infection can develop as parts of dead, scarred pancreas are reabsorbed by the body.
- Diabetes: When you have pancreatitis, your body uses blood sugar differently. This can lead to diabetes.
- Pancreatic cancer: A pancreas that is constantly inflamed or even scarred is at greater risk of developing cancer.
- Malnutrition: Despite eating what you always have eaten, you may notice significant weight loss if you have pancreatitis. That’s because you’re not absorbing nutrients properly due to your pancreatitis.
- Kidney failure: For some, kidney failure accompanies pancreatitis. This can be treated with dialysis during periods of acute pancreatitis.
- Difficulty breathing: When your pancreas doesn’t do its job properly, your body’s chemical makeup changes. You end up not having enough oxygen in the body and can develop breathing problems.
Pancreatitis Diagnosis
Diagnosing acute pancreatitis typically starts with a blood test that tests for high levels (typically 3 times higher than normal) of two digestive enzymes: amylase and lipase. If the diagnosis remains unclear, the doctor may order one or more of the following tests:
- Pancreatic function test: To determine if the pancreas is churning out the appropriate amount of digestive enzymes.
- Glucose tolerance test: To ascertain damage to pancreas cells responsible for producing insulin.
- Transabdominal ultrasound: To check for gallstones, which are the most common cause of acute pancreatitis.
- Computerized tomography (CT) and magnetic resonance imaging (MRI): To determine how severe the pancreatitis is using imaging technology.
- ERCP, or endoscopic retrograde cholangiopancreatography: To get a more detailed picture of the bile ducts and pancreatic duct using x-rays, although it’s a much more invasive procedure, as it requires inserting a thin tube through the mouth and down into the stomach.
- Biopsy: To remove a small tissue sample from the pancreas for analysis under a microscope.
Pancreatitis Treatment
An acute pancreatitis diagnosis is usually treated with IV fluids for hydration and pain medications to alleviate discomfort. In cases of severe acute pancreatitis, patients are admitted to the intensive care unit (ICU) in order to monitor damage to the heart, lungs, or kidneys. Severe pancreatitis can kill pancreatic tissues, and surgery to remove the damaged tissue may be required. Expect the following:
- No food for 2 days: The first thing a doctor will tell you if you have pancreatitis is to stop eating for 48 hours. The pancreas needs to “relax,” so to speak, and the inflammation needs to subside before food can be reintroduced.
- Intravenous fluids for hydration: As your body tries to right the pancreas, it needs extra fluids.
- ERCP surgery: The ERCP can remove blockages caused by gallstones without the need for invasive, full-blown surgery.
- Surgery on the gallbladder or pancreas: If gallstones are severe, your doctor may suggest you have your gallbladder removed. Sometimes surgery is needed on the pancreas to drain fluid or remove dead tissue. If surgery is called for, you can accelerate healing with Heal, an amino acid therapeutic proven to improve recovery times and surgical outcomes.
Treatment for Pain
Pancreatitis pain is severe. Your doctor may refer you to a pain specialist or even recommend surgery to block pain-transmitting nerves.
There is a high risk of developing an addiction to opioid narcotics commonly prescribed for pancreatitis pain. Other pain management tools, particularly for chronic pancreatitis, such as meditation, yoga, massage, and acupuncture, should also be considered when devising a pancreatitis treatment plan.
A small clinical trial in 2007 showed yoga improved the lives of people with chronic pancreatitis. The study, published in the World Journal of Gastroenterology, showed the 30 people randomized to yoga treatment reported less stress and even cut down on drinking. And a small 2006 in the journal Gut showed yoga helped people with chronic pancreatitis manage pain and anxiety.
Treating Pancreatitis with Natural Prevention Methods
Pancreatitis is an incredibly dangerous and potentially fatal condition. Attempting to treat pancreatitis at home homeopathically could result in death. If you have the symptoms of pancreatitis, see a doctor. To help keep your pancreas healthy, implement the dietary suggestions below.
- Fill up on plenty of antioxidants, which are found in colorful fruits and vegetables. There are some indications that treating pancreatitis with antioxidants may be beneficial, although more clinical trials are needed, according to a systematic review published in 2008 in the World Journal of Gastroenterology.
- Add a turmeric supplement. In an animal model in a laboratory, scientists have seen how turmeric suppresses a molecular pathway needed for inflammation. The study appeared in Medical Science Monitor. In a different study involving a mice model in a laboratory, turmeric inhibited pancreatic cancer cell growth. The study appeared in the journal BioMed Research International.
- Quit smoking. Smoking sends free radicals sailing through the body, which only feed inflammatory conditions. A 2013 study published in the journal Gastroenterology on the epidemiology of pancreatitis and pancreatic cancer concluded quitting smoking was the single best way to reduce the risk of cancer of the pancreas.
- Quit drinking. Alcohol is deadly for people with pancreatitis. In fact, alcoholism is one of the major causes of pancreatitis. Although the mechanism of action remains unclear, authors of a 2008 paper printed in the World Journal of Gastroenterology said combining smoking and drinking seems to create a synergistic effect to heighten pancreatitis risk even further.
- Be mindful about staying hydrated. A troubled pancreas robs the body of water due to digestive problems such as diarrhea. It’s important to replace it.
- Avoid high-fat foods and eat plenty of fruits and vegetables. These foods are easy on your pancreas and help keep it healthy.
By avoiding alcohol and cigarettes and by eating a healthy diet, most people can obvert ever having an acute pancreatitis attack. But it’s important to know that if you ever feel that sharp abdominal pain in the back of your upper abdomen, and it’s radiating up your back and not going away, you need to see a doctor right away.

Up to 25% off Amino
Shop NowTAGS: conditions
Join the Community
Comments (0)
Most Craveable Recipes




 833-264-6620
833-264-6620



















