Signs of Colon Cancer and the Importance of Early Screening
 By: by Amino Science
By: by Amino Science

“I’m too young for colon cancer,” is a common refrain, but it also demonstrates the misconception many people have about this potentially deadly disease, as colon cancer, or colorectal cancer, is often thought of as an “elderly” cancer—a cancer that doesn’t affect people at a younger age. While it’s true that most cases of colon cancer occur after age 50, the condition can develop at any age, particularly in those with a family history of the disease. But what are the signs of colon cancer, what’s the recommended age to start screening for the disease, and how do you know if you should be screened early?
Signs of Colon Cancer
According to the American Cancer Society, colon cancer is the third leading cause of cancer-related deaths in adults in the United States, and more than 100,000 new cases are estimated to be diagnosed in 2019.
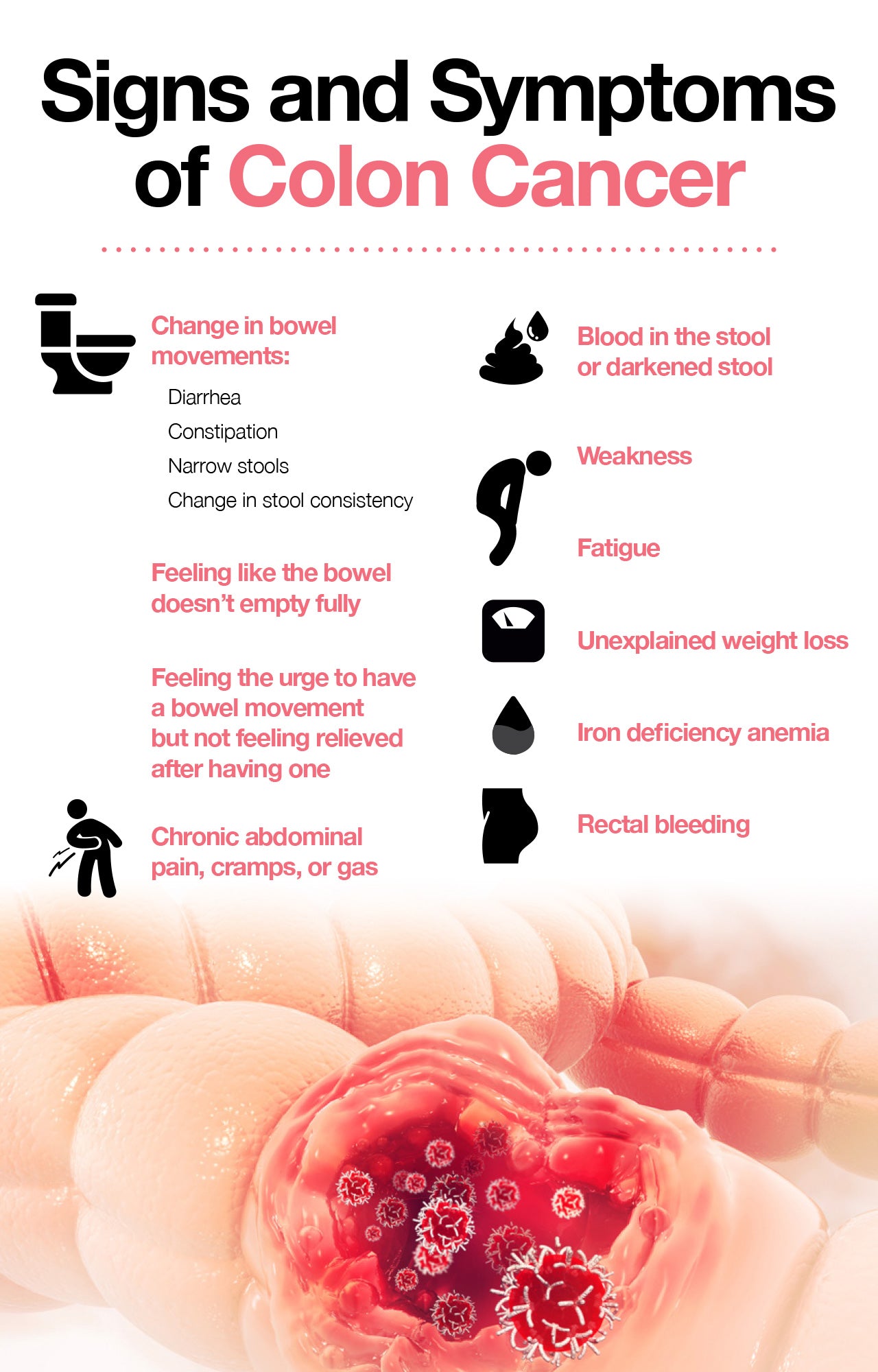
Despite the fact that symptoms of colon cancer don’t always appear in the early stages of the disease, symptoms do occur, though they may differ based on the size and location of the cancer. However, typical warning signs to look out for include:
- Change in bowel habits
- Rectal bleeding
- Fatigue
- Unexplained weight loss
- Persistent abdominal pain
- Iron deficiency anemia
Because colon cancer symptoms may be vague or overlap with other conditions, such as irritable bowel syndrome (IBS) or ulcerative colitis, regular screenings are important for ruling out other causes.
Colon Cancer Screening
Like other cancers, early detection is key when it comes to treating colon cancer because the earlier the cancer is found, the better the odds of beating it. And cancer caught via early screenings often has the best outcome, as it usually hasn’t had a chance to spread to other parts of the body.
In addition, the majority of colon cancer cases develop from colon polyps, which don’t always present with symptoms, so screening to check for them is crucial for diagnosing colon cancer early.
The Centers for Disease Control and Prevention (CDC) recommends that regular colon cancer screenings begin at age 50 in those who aren’t at increased risk of developing colon cancer. However, the American Cancer Society recommends that those at average colon cancer risk begin regular screenings at age 45.
Given this difference in opinion, it’s best to discuss what age is right for you with your health care provider.
However, once regular screenings begin, both the CDC and the American Cancer Society recommend they continue up to age 75. After that, and until the age of 85, the American Cancer Society recommends that the decision to be screened be based on personal preference, life expectancy, overall health, and prior screening history. After the age of 85, colon cancer screening is no longer required.
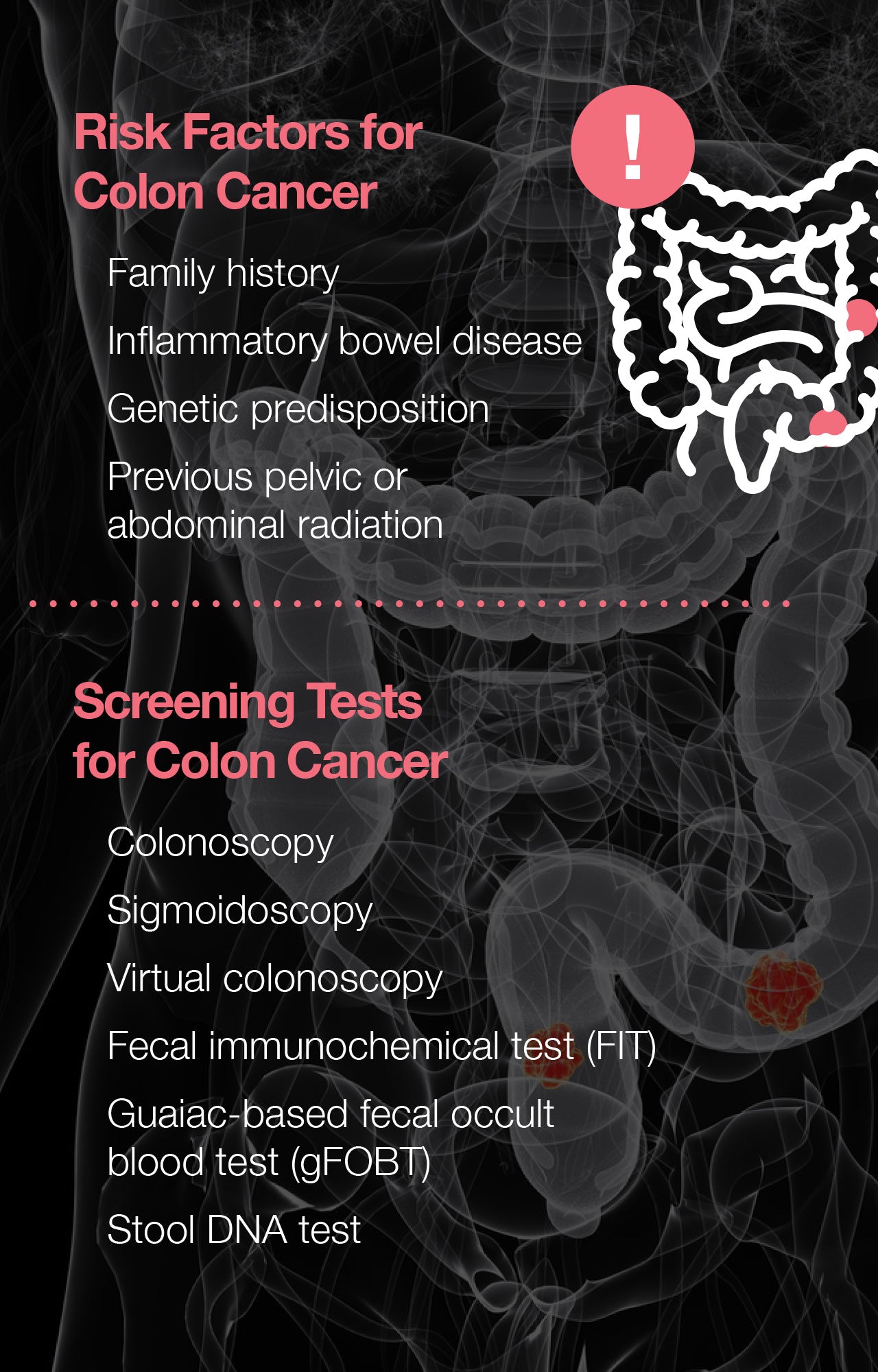
Early screening may also be recommended in people younger than 50 when they have a higher than average risk of developing colon cancer. Risk factors that may call for early or more frequent colon cancer screening include:
- Family history: People with close relatives who’ve had colorectal polyps or a cancer diagnosis have a greater chance of developing colon cancer.
- Pre-existing conditions: People diagnosed with an inflammatory bowel disease, such as ulcerative colitis or Crohn’s disease, have an increased risk of developing colorectal cancer.
- Genetics: Certain hereditary syndromes, including familial adenomatous polyposis (FAP) and Lynch syndrome, or hereditary nonpolyposis colorectal cancer (HNPCC), put one at a higher risk of developing colon cancer.
- Radiation: Those who’ve had radiation to the abdomen or pelvic area to treat previous cancers have an increased risk of colorectal cancer.
If you’re under the age of 50 and have any of the above risk factors, you should speak with your doctor about beginning early colorectal cancer screenings.
Types of Colon Cancer Screenings
Depending on a person’s cancer risk, the type of colon cancer screening recommended may be either invasive or noninvasive. However, the test offered will be one of two types:
- Visual
- Stool-based
Visual Tests
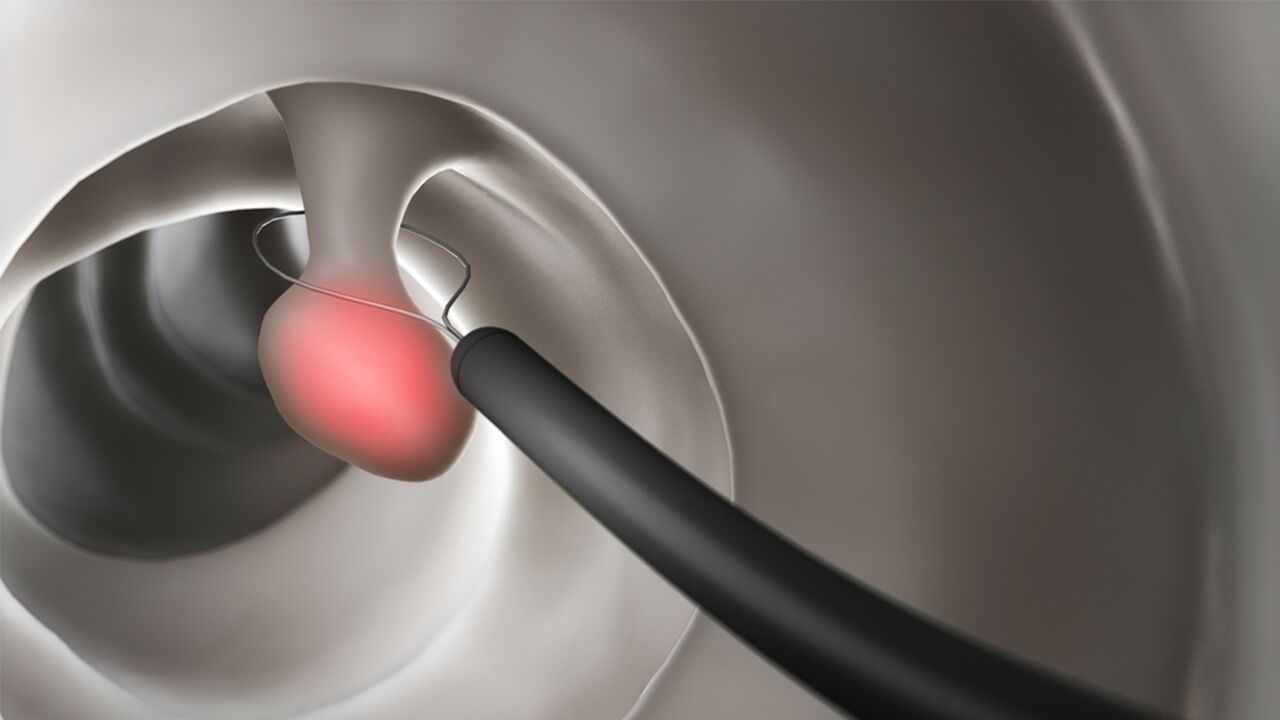
Visual colon cancer tests are usually invasive, as they involve instruments designed to examine the inside of the colon for any abnormalities, including polyps or suspicious-looking areas that may need to be biopsied or removed.
Common visual exams include:
- Colonoscopy: During a colonoscopy, the rectum and entire length of the large intestine are examined with the use of a flexible fiber-optic instrument called a colonoscope. If no suspicious findings are noted, those at average risk will most likely be recommended follow-up exams every 10 years.
- Sigmoidoscopy: During a sigmoidoscopy, a flexible tube called a sigmoidoscope is used to examine the rectum and lower part of the colon. If nothing abnormal is found, follow-up exams may be performed every 5 years in those at average risk.
- Computed tomography (CT) colonography: This virtual colonoscopic exam is the noninvasive alternative to traditional colonoscopy. Utilizing a CT scan to examine the colon and rectum, CT colonography is as effective at catching abnormalities as a traditional colonoscopy but is noninvasive and requires no anesthesia. However, the test does use low doses of radiation, and in situations where polyps or other abnormal findings are noted, a traditional colonoscopy is required for removal or biopsy. Otherwise, follow-up exams may be performed every 5 years in those at average risk.
Stool-Based Tests
If your health care provider agrees you’re a suitable candidate, noninvasive testing in the form of a stool test may be chosen to look for signs of colon cancer. However, unlike a colonoscopy, sigmoidoscopy, or CT colonography, stool tests need to be performed much more frequently.
Common stool-based exams include:
- Fecal immunochemical test (FIT): This test, which is also known as an immunochemical fecal occult blood test (iFOBT), detects occult (hidden) blood in the stool by reacting to the presence of hemoglobin, a component of red blood cells. The FIT is performed by collecting small samples of stool on cards or in tubes. The test can be conducted in a person’s own home but must be performed every year.
- Guaiac-based fecal occult blood test (gFOBT): The gFOBT is performed in an individual’s own home using a kit that allows a person to check more than one stool sample. Unlike the FIT, the gFOBT comes with certain drug and dietary restrictions, including the avoidance of nonsteroidal anti-inflammatory drugs (NSAIDs), vitamin C, and red meat for several days before performing the test. Like the FIT, the gFOBT must also be performed every year.
- Stool deoxyribonucleic acid (DNA) test: Also known as a multitargeted stool DNA test, or MT-sDNA, this exam checks stool for abnormal sections of DNA related to polyp or cancer cells. The only product currently on the market that offers this type of screening is Cologuard, which also tests for blood in the stool. The stool DNA test can be performed every 3 years in those at average risk.
Colorectal cancers that are caught early are associated with the best outcomes and have a 5-year survival rate of approximately 90%. If you’re nearing 50 or have personal risk factors or a history of colon cancer in one or more of your family members, you should speak with your health care provider about getting screened. To optimize your health as you grow older, consider taking an essential amino acid supplement.

Up to 25% off Amino
Shop NowTAGS: conditions
Join the Community
Comments (0)
Most Craveable Recipes



 833-264-6620
833-264-6620



















