What Is Ulcerative Colitis: Causes, Symptoms and Treatments
 By: by Amino Science
By: by Amino Science

There are many diseases that can affect the gastrointestinal system, from irritable bowel syndrome to Crohn's disease, but ulcerative colitis is one of the most debilitating. According to the Crohn’s and Colitis Foundation of America, 1.6 million Americans have inflammatory bowel disease, and ulcerative colitis affects 907,000 of them. How does ulcerative colitis differ from other digestive disorders, and what exactly is ulcerative colitis?
Ulcerative colitis is a chronic inflammatory disease that affects the large intestine and rectum and causes long-lasting inflammation and ulcers in the digestive tract. Symptoms usually develop over time and may lead to life-threatening complications.
Complications of ulcerative colitis can include swelling of the colon (toxic megacolon), a hole in the colon, bone loss, blood clots, colorectal cancer, and even liver disease.
Ulcerative Colitis Causes
The cause of ulcerative colitis is unknown. Doctors used to suspect that diet and stress were responsible for the disease, but they now believe that diet and stress are not the cause but can indeed make the disease worse.
Immune system malfunction is considered a possible cause, because when the immune system reacts to an invasion, it attacks the cells in the digestive tract. Mistaking food and gut bacteria as invaders, white blood cells proliferate in the lining of the colon, causing chronic inflammation and ulcers.
Despite the lack of consensus on a precise cause, risk factors may include age, race or ethnicity, and family history (you may be at risk if you have a close relative who has or had the disease).
Ulcerative colitis usually affects people before the age of 30, and Caucasians are more likely to develop this condition.
Ulcerative Colitis Symptoms
The symptoms of ulcerative colitis depend on the level of inflammation, and they are classified according to location.
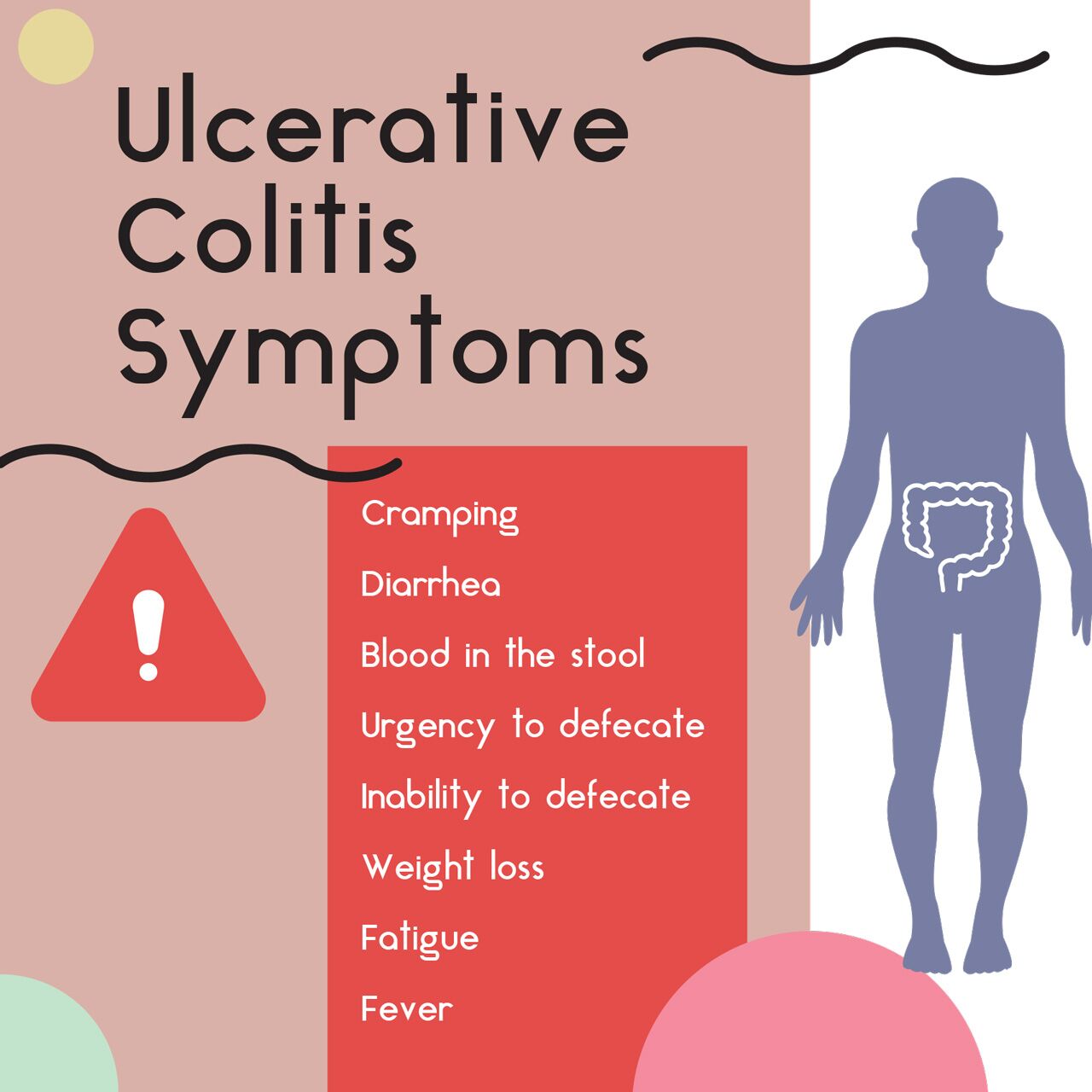
The most common symptoms of ulcerative colitis include:
| Bloody diarrhea | Abdominal pain |
| Cramps | Bloody stool |
| Rectal pain | Urgent need to defecate |
| Inability to defecate | Unexplained weight loss |
| Joint pain | Tiredness |
| Fever | Stunted growth in children |
Types of Ulcerative Colitis
- Ulcerative proctitis: The mildest form of ulcerative colitis, ulcerative proctitis is characterized by rectal bleeding and inflammation in the region closest to the rectum.
- Proctosigmoiditis: Here, the inflammation occurs in the rectum and sigmoid colon. Symptoms are typically bloody stool, abdominal pain, and inability to produce bowel movements but with the strong urge to do so.
- Left-sided colitis: The inflammation that occurs with left-sided colitis travels to the descending colon and results in bloody diarrhea, abdominal cramping on the left side, and weight loss.
- Pancolitis: This type of ulcerative colitis inflames the entire colon. Symptoms may be more intense and weight loss drastic.
- Acute severe ulcerative colitis: The rarest type of colitis, it's acute, severe, and affects every part of the colon.
Your health care provider will use blood tests to check for signs of anemia or infection and a stool sample to diagnose ulcerative colitis. To investigate further, your doctor may order a colonoscopy, a more invasive exam that allows for a view of the entire colon using a thin, lighted tube with an attached camera.
If the colon is too inflamed for a colonoscopy, your doctor with opt for a flexible sigmoidoscopy to examine your rectum and colon. If a complication is suspected, a CT scan may be ordered, and if symptoms are especially pronounced, your physician may take an X-ray to rule out a condition such as a perforated colon.
Ulcerative Colitis Treatment Options
The type of treatment depends on the severity of the condition—and it may take time to find a medication that helps because not everybody reacts in the same way to drugs. It is crucial to follow your doctor’s directions because many of these drugs have side effects. You can also check out this article on the best and worst foods to eat for ulcerative colitis to help manage your symptoms.
Anti-Inflammatory Drugs
Anti-inflammatory drugs include 5-aminosalicylates (the primary choice for mild to moderate ulcerative colitis) such as sulfasalazine (Azulfidine), mesalamine (Asacol HD, Delzicol, others), balsalazide (Colazal), and olsalazine (Dipentum). Corticosteroids are generally used in cases of severe ulcerative colitis that don’t respond to other treatments—these drugs have strong side effects, so long-term use is not recommended.
Immune System Suppressors
These drugs help lower inflammation, but they also suppress the immune system response. The most common immunosuppressant drugs include Azathioprine (Azasan) and mercaptopurine (Purinethol). Cyclosporine (Gengraf) is usually prescribed to people who have had issues with other medications. This drug has serious side effects and is not for long-term use.
Drugs such as infliximab (Remicade) neutralize a protein produced by your immune system, and they are usually proscribed for those with severe ulcerative colitis who have had issues with other treatments.
Other Medications
Antibiotics are usually prescribed to ulcerative colitis sufferers running a fever. Anti-diarrheal medications (Imodium) may be effective for severe diarrhea. Pain relievers such as acetaminophen (Tylenol) may be used. Do not use ibuprofen (Advil), naproxen sodium (Aleve), and diclofenac sodium (Voltaren), which can exacerbate symptoms. Iron supplements can help manage anemia in patients with chronic intestinal bleeding.
Surgery
Surgery can be effective in eliminating ulcerative colitis, but the procedure removes the rectum and the entire colon. The surgeon constructs a pouch from the end of the small intestine and attaches it directly to the anus, allowing the patient to expel waste without using a bag to collect stool.
It is important to mention that patients with ulcerative colitis are at higher risk of developing colon cancer. Frequent screenings are recommended. If the disease goes beyond the rectum, a surveillance colonoscopy should be done every 1 to 2 years.
How to Treat Ulcerative Colitis with Amino Acids
Studies suggest that L-arginine, a nonessential amino acid known to keep the immune system strong, can help patients who have ulcerative colitis. In a rat model, L-arginine supplementation healed the intestinal mucosa. Another test analyzed the effect of L-arginine on patients with histologically-proven pancolitis. The experiment showed that L-arginine concentration may prove to be useful as a biomarker for ulcerative colitis disease severity.
More generally, ulcerative colitis patients are at risk of nutrient depletion, particularly during an inflammatory flare-up. To counter this, the European Society for Enteral and Parenteral Nutrition recommends an increase in dietary protein intake to a level as much as twice the recommended dietary allowance for healthy individuals in order to maintain muscle mass and function. This level of intake may be impractical to achieve, and complete digestion may be limited.
Adding an essential amino acid supplement to the diet may provide important beneficial effects. When provided in free form, amino acids are fully digested in the small intestine and therefore act locally through the luminal side via the bloodstream to reach mucosal sites distant from the sites of absorption. Amino acid supplementation has been shown to provide beneficial effects on the inflammatory response, oxidative stress reactions, and other favorable effects in the gut. In addition, supplementation with essential amino acids will help to maintain muscle mass and metabolic health.
You can shop for the best amino acids for ulcerative colitis here.



 833-264-6620
833-264-6620


















