What Is Uveitis: Symptoms, Causes, Treatments
 By: by Amino Science
By: by Amino Science
What is uveitis?
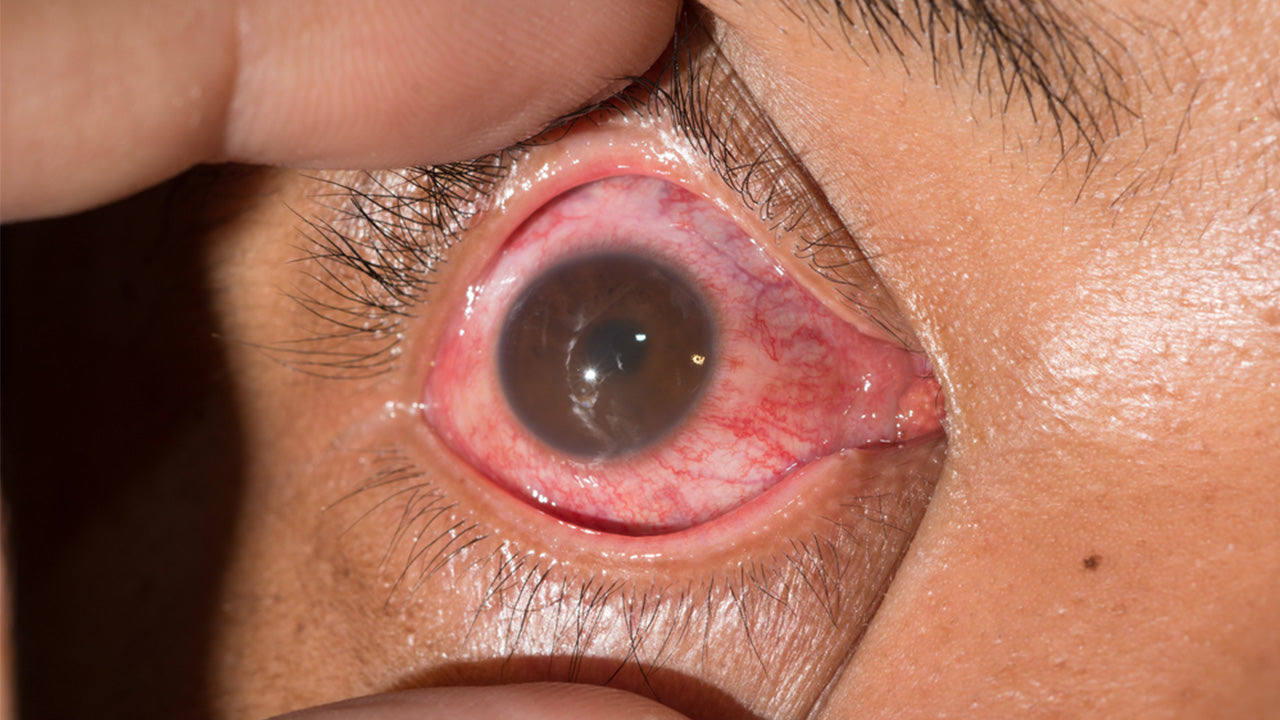
A form of eye inflammation, uveitis is a condition that affects the uvea, which is the middle layer of tissue in the eyewall. The uvea is made up of the iris, the ciliary body, and the choroid, and contains a vast matrix of blood vessels that support the health of the eye. Uveitis can damage vital eye tissue, leading to permanent vision loss.
Occurring in one or both eyes, inflammation of the uvea can spread from the middle layer of the eye to other parts of the eye, including the cornea, retina, and optic nerve, and lead to blurred vision and other unpleasant symptoms. While not typically serious, left untreated uveitis can result in permanent loss of vision. For this reason, all eye disorders should be evaluated promptly by an ophthalmologist. By understanding the symptoms and causes of this condition, you can determine if and when to seek treatment in order to protect your eye health for the long term.
Types of Uveitis (Plus Symptoms)
Named because it often affects a part of the eye called the uvea, uveitis causes a number of symptoms that can affect patients’ vision and overall health. Signs of uveitis in one or both eyes include:
- Eye redness
- Eye pain
- Sensitivity to light
- Blurry vision
- Floaters or dark spots in the field of vision
- General vision issues and concerns
While some symptoms of uveitis come on suddenly, others develop gradually and worsen with time. The symptoms of the condition also vary based on the type of uveitis.
The most common form of uveitis, acute anterior uveitis accounts for swelling toward the front of the eye and can cause eye pain, vision blurring, small pupils, and light sensitivity. With intermediate uveitis, floaters or blurred vision are common signs. In cases of posterior uveitis in which inflammation and swelling occur in the back of the eye, vision loss may occur. Most common in young men, pars planitis is a type of uveitis that affects the narrowed area (pars plana) between the iris and choroid. The condition can be linked to multiple sclerosis in patients older than 25.
While some patients suffer from an acute case of uveitis, others develop a chronic form of the condition that can recur many times over the years.
Uveitis Causes
There’s no one cause of uveitis. A term for a group of inflammatory diseases that affect eye tissue, uveitis can occur as a result of an underlying eye problem or in conjunction with an inflammatory condition such as an autoimmune disorder. Conditions such as rheumatoid arthritis and ankylosing spondylitis cause the immune system to launch an attack against healthy tissue. The issue can strike patients of any age, but it is most common in adults between 20 and 60.
While doctors are unable to determine the cause of uveitis in about 50% of cases, the condition may stem from any of the following:
- Undergoing eye surgery or suffering an eye injury
- Being diagnosed with an autoimmune disorder, such as sarcoidosis
- Suffering an inflammatory disorder, such as Crohn’s disease
- Contracting an infection like cat-scratch disease, herpes zoster, or syphilis
- Developing certain cancers that affect the eye, such as lymphoma
- Smoking cigarettes
With treatment, healthy uveitis patients have an excellent prognosis. However, if the condition is not addressed quickly, it can lead to complications such as glaucoma, cataracts, damage to the optic nerve, and retinal detachment. In rare cases, patients may suffer permanent vision loss. For this reason, it’s important that you seek immediate care if you think you may be suffering from uveitis.
Methods for Uveitis Treatment
The goal of uveitis treatment is to resolve inflammation while alleviating pain. If tissue damage has occurred, doctors will also strive to prevent further damage and restore lost vision. The medication that’s prescribed depends in large part on the patient’s specific symptoms. Some of the most commonly recommended uveitis treatments include corticosteroid eye drops, injections in or around the eye, and immunosuppressive drugs. The latter treatment is often used when the disease occurs in both eyes.
While steroidal anti-inflammatory medications are typically effective in treating uveitis, long-term steroid use comes with significant side effects. In rare cases, patients may suffer stomach ulcers, osteoporosis, and diabetes. Weight gain and fluid retention are also common. In most cases, doctors don’t recommend taking steroids for uveitis for longer than 3 months.
Additionally, your ophthalmologist may recommend immunosuppressive agents such as methotrexate, mycophenolate, azathioprine, and cyclosporine.
In more serious cases of uveitis, your doctor may recommend surgical intervention. The goal of treatment is to temporarily replace the gel-like vitreous humor (the tissue that fills the eyeball behind the lens) with air or gas and install a device that will slowly release corticosteroids over time. The vitreous will replace itself. Typically, this method is recommended only for patients with severe uveitis or those whose condition is caused by certain infections. You can accelerate healing with essential amino acids. Discover how here.
It’s not uncommon to experience pain or discomfort while being treated for uveitis. Wearing dark glasses and taking OTC painkillers can help you feel better. Ask your doctor about additional options for alleviating symptoms.
Among working adults, uveitis is one of the leading causes of blindness in the U.S and the world. Regular visits to an eye doctor are among the best ways to protect your vision and your health in the coming years.


Up to 25% off Amino
Shop NowTAGS: conditions
Join the Community
Comments (0)
Most Craveable Recipes




 833-264-6620
833-264-6620



















