What Is Celiac Disease and Is There a Cure?
 By: by Amino Science
By: by Amino Science

Celiac disease is an autoimmune disorder in which the immune system attacks the small intestine and causes problems with nutrient absorption. While the condition is estimated to affect approximately 1% of people in the United States, the Celiac Disease Foundation states that around 2.5 million Americans are unaware they have the condition and are therefore at risk of long-term health problems. But what causes celiac disease, and is there a cure? In this article, we’re going to take a look at these questions and uncover all you need to know about this potentially serious autoimmune disease.
What Causes Celiac Disease?
Celiac disease, also known as celiac sprue, is caused by an overactive immune response to gluten—a protein found in many cereal grains. Over a period of time, this hyperactive immune response, and the gluten intolerance it provokes, can damage the finger-like projections of the lining of the small intestine.
Unfortunately, these projections, which are called villi, are responsible for absorbing many of the nutrients in the foods we eat, and their inability to function normally can lead to a number of negative health consequences.
While the exact factors involved in the development of celiac disease are unknown, there is a clear hereditary basis for the disease. In fact, people who have an immediate family member with celiac disease have about a 10% chance of developing the condition themselves.
Types of Celiac Disease
According to the World Gastroenterology Organization, celiac disease can be divided into two types.
- Classical celiac disease: In people with this type, signs of malabsorption are readily apparent and may include chronic diarrhea, fatty stools (steatorrhea), growth retardation, and weight loss.
- Non-classical celiac disease: This type of celiac disease is much more difficult to diagnose, as signs of malabsorption may be vague, and symptoms may affect more than just the digestive system. For example, people with non-classical celiac disease may experience iron deficiency anemia, fatigue, migraines, tingling or numbness in the hands or feet, dental enamel defects, depression, anxiety, and dermatitis herpetiformis—an itchy skin rash that’s caused by gluten sensitivity but may present with no other symptoms.
In addition, people with celiac disease may suffer from an asymptomatic form of the condition called silent celiac disease. While people with silent celiac disease don’t complain of symptoms, they still experience intestinal damage.
Risk Factors for Celiac Disease
Certain factors may put a person at greater risk of developing celiac disease. Some of these include:
| Eating gluten prior to 6 months of age | Frequent rotavirus infections |
| Down syndrome | Turner syndrome |
| Autoimmune thyroid diseases | Rheumatoid arthritis |
| Microscopic colitis | Inflammatory bowel disease |
| Addison’s disease | Type 1 diabetes |
Symptoms of Celiac Disease
Celiac disease affects people differently, so diagnosis can be difficult. In addition, almost 300 different symptoms have been found to occur with celiac disease, and symptoms may vary based on whether the illness begins in childhood or adulthood. Some of the more common symptoms in children include:
- Chronic diarrhea or constipation
- Abdominal pain
- Bloating
- Flatulence
- Weight loss
- Growth problems
- Attention-deficit/hyperactivity disorder (ADHD)
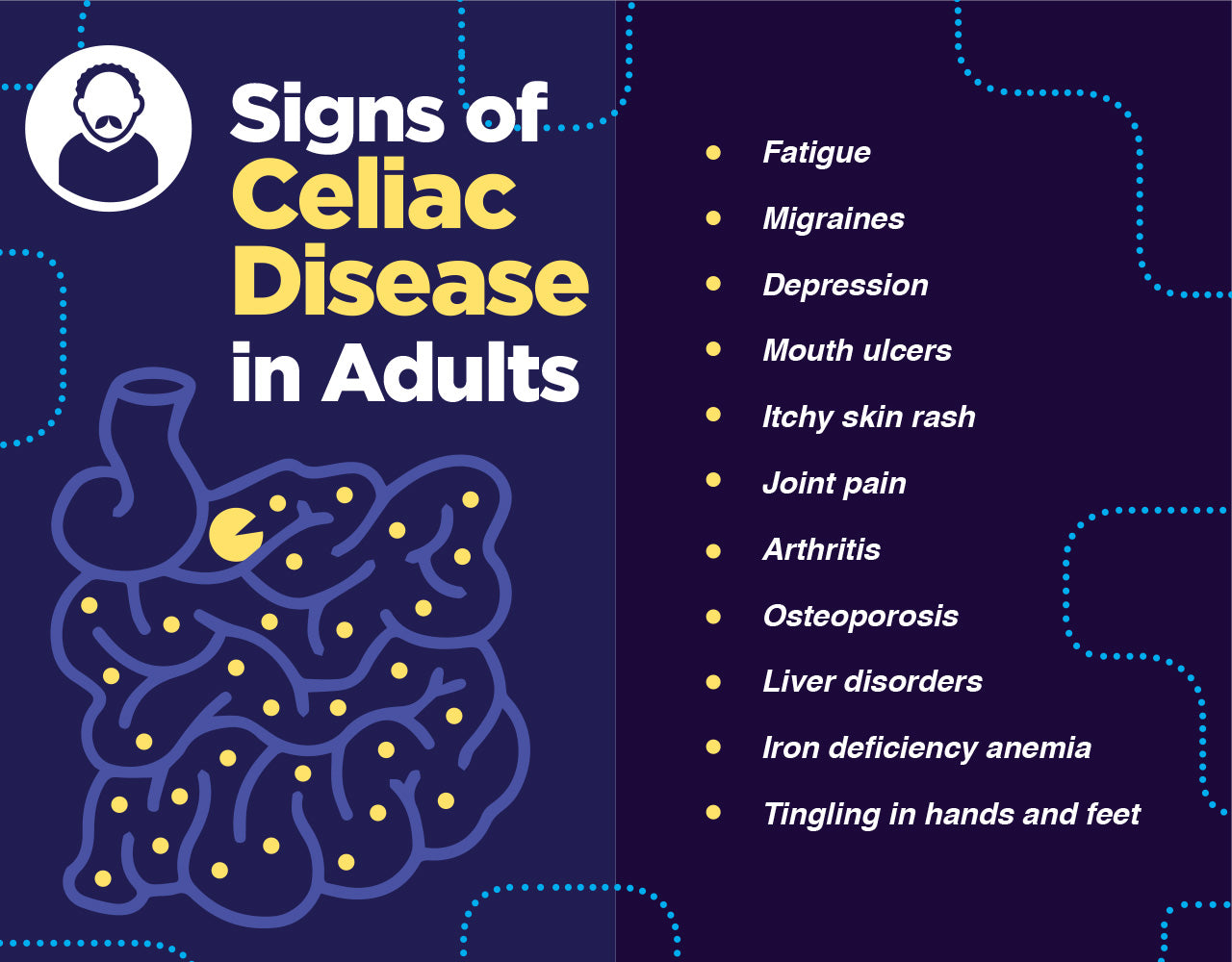
By contrast, adults with celiac disease are much less likely to experience digestive disorders. Symptoms more common in adults include:
- Iron deficiency anemia
- Dermatitis herpetiformis
- Oral ulcers
- Osteoporosis
- Joint pain
- Headaches
- Fatigue
- Cognitive impairment
Complications of Celiac Disease
If celiac disease isn’t properly treated, it can lead to serious complications, including:
- Osteomalacia
- Osteoporosis
- Reproductive problems
- Lactose intolerance
- Gastrointestinal cancers
- Seizures
Diagnosing Celiac Disease
If you’re experiencing signs and symptoms of celiac disease, your health care provider can confirm the condition by performing a blood test to evaluate for the presence of antibodies to gluten. In addition, genetic testing to look for genes known to be associated with celiac disease can be conducted.
If the results of these tests are positive, your health care provider may then decide to perform an endoscopy to examine the lining of the small intestine for signs of damage.
Treatment of Celiac Disease
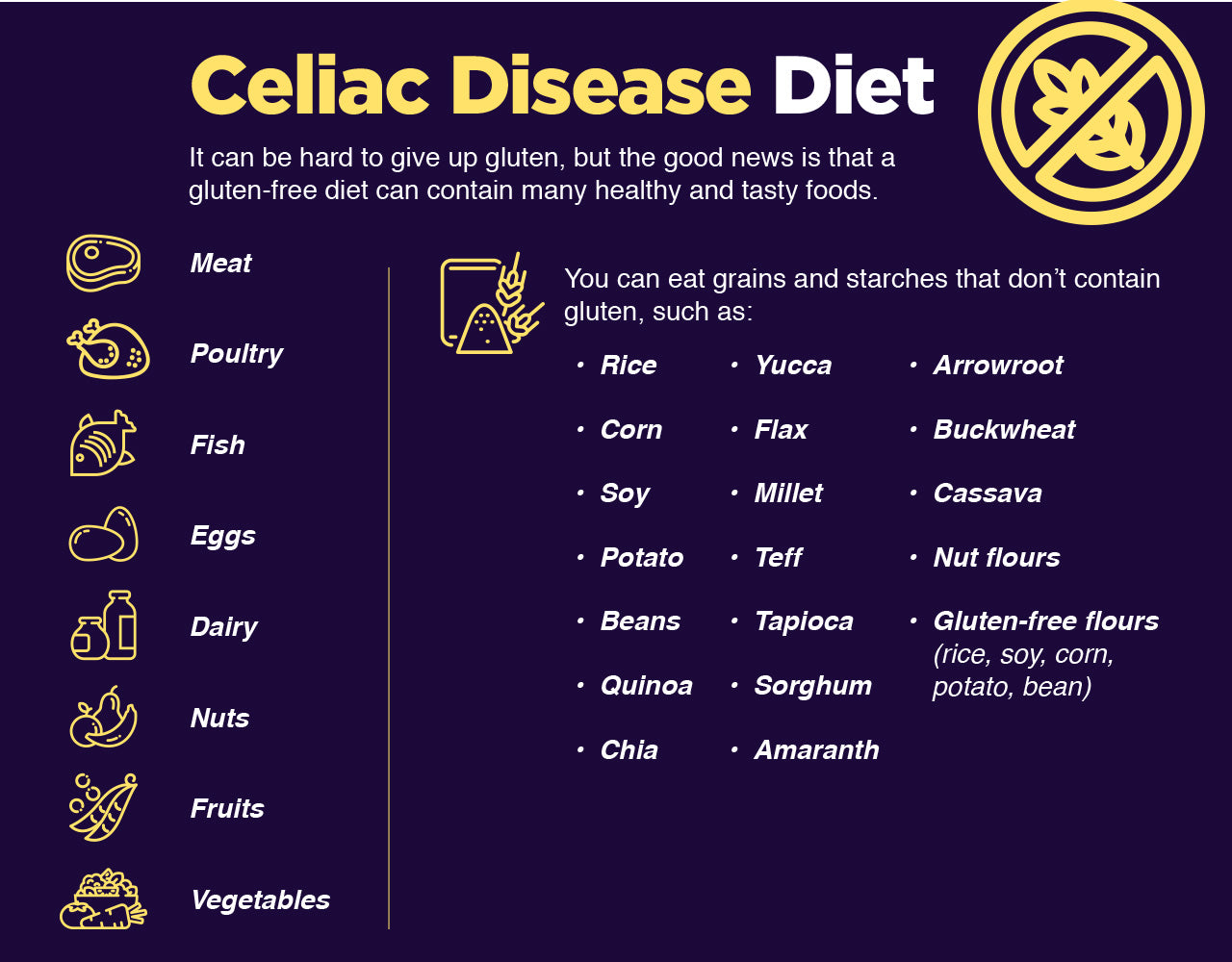
Unfortunately, there’s currently no cure for celiac disease. So if you’ve been diagnosed with the condition, it’s important to understand that the best—and only—way to successfully manage it is by eating a strict gluten-free diet. But before you begin your journey to gluten-free foods, you first need to identify and eliminate the gluten-containing foods you’ve been eating. These may include:
- Wheat
- Barley
- Bulgur
- Durum
- Rye
- Spelt
- Triticale
Removing gluten from your diet not only gets rid of the source of inflammation, but it also allows the villi in your small intestine to heal. However, even though these changes may cause you to feel better in just a couple of weeks, it may take 6 months or more for the villi to completely heal.
It’s also vital to remember that going gluten free isn’t just about your diet. Unfortunately, gluten may be found in a number of non-food items, too, including:
- Medications
- Preservatives
- Vitamin and mineral supplements
- Herbal supplements
- Lip products
- Toothpaste
- Envelope glue
Moreover, some alcohol—especially beer—and many processed foods contain gluten as a hidden ingredient, so make sure you avoid these types of products unless they’re clearly labeled gluten free.
And be sure to read the label before buying anything. Even if a product doesn’t explicitly say it’s gluten free, it may list common allergens, which can help you figure out if gluten is present. In addition, checking the list of ingredients for obvious offenders can help you determine whether gluten might be an issue.
When in doubt, err on the side of caution and don’t buy the product. After all, there are many gluten-free alternatives available. And if you can’t find what you’re looking for at your local grocery store, there’s a variety of stores online that can help you find what you need.
Also keep in mind that certain gluten-free grains, such as oats, may be contaminated with gluten-containing grains during growing and processing. So while oats, for example, aren’t generally harmful for most people with celiac disease, it’s best to avoid them unless they’re specifically labeled gluten free.
If you’ve been diagnosed with celiac disease and follow a strict gluten-free diet, you should find that your symptoms gradually dissipate and your health improves. However, a small number of people with refractory celiac disease don’t respond to dietary changes. So if your symptoms don’t improve within several weeks—or worsen—be sure to see your health care provider for further follow-up and testing.
To make sure you are not suffering nutrient depletions in the protein department due to dietary restrictions, consider supplementing with essential amino acids.

Up to 25% off Amino
Shop NowTAGS: conditions
Join the Community
Comments (0)
Most Craveable Recipes




 833-264-6620
833-264-6620




















