What Is Whooping Cough and Is It Contagious?
 By: by Amino Science
By: by Amino Science

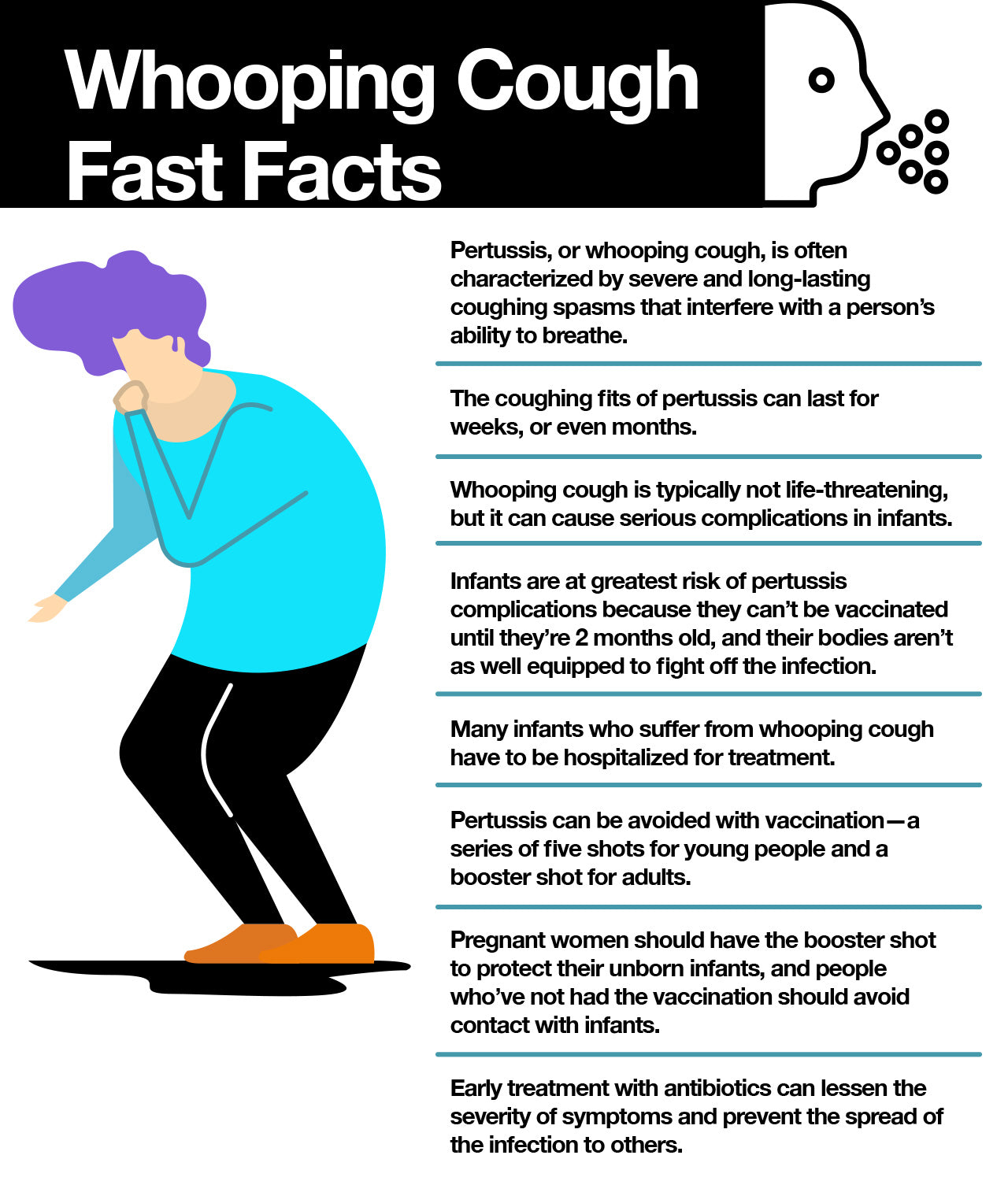
Whooping cough may seem like an illness from another time, but this respiratory infection known for its uncontrollable, violent coughing fits that can make it hard to breathe is making a comeback. And though it seldom causes serious complications, it can be harmful—and even fatal—to certain segments of the population. In this article, we’re going to take a look at this blast from the past and dig into exactly what whooping cough is, why it’s on the rise again, and what you need to do to protect yourself and those you love.
What Is Whooping Cough?
Whooping cough, whose scientific name is actually pertussis, is a respiratory infection caused by bacteria called Bordetella pertussis. Similar bacteria called Bordetella parapertussis also cause a pertussis-like illness but have milder (or no) symptoms and do not produce the pertussis toxin.
Bordetella pertussis bacteria cause the symptoms of whooping cough by attaching to the tiny, hair-like extensions (cilia) that line part of the upper respiratory tract, where they release toxins that damage the cilia and cause the airways to swell.
Pertussis is known as whooping cough because of the whooping sound many people make when they inhale sharply after a coughing fit to catch their breath. The condition is also known colloquially as the 100-day cough because the infection can last for weeks, or even months.
Is Whooping Cough Contagious?
We’re pretty sure you already know the answer to this one. But in case you don’t, the answer is a resounding yes.
Whooping cough is a highly contagious bacterial infection that’s spread from person to person by coughing, sneezing, and breathing (it really can be spread by the breath of an infected person). In fact, the Centers for Disease Control and Prevention (CDC) states that almost everyone who isn’t immune to whooping cough will get sick if they’re exposed to it. This includes infants, many of whom contract the illness from their older siblings, parents, or caregivers.
People infected with whooping cough are most contagious up to about two weeks after the cough begins, though antibiotics may shorten the amount of time a person is able to pass the infection on to others.
Symptoms of Whooping Cough
After a person is exposed to pertussis, symptoms usually develop within 5 to 10 days, but they may take as long as 3 weeks to emerge. The illness normally begins with cold-like symptoms, such as a runny nose and sneezing—and possibly a mild cough or low-grade fever—which is why health care professionals often don’t suspect whooping cough when it’s in its early stages.
However, after 1 to 2 weeks, symptoms may progress to paroxysms of severe coughing that result in the stereotypical “whoop.” These coughing spells tend to occur more often (and at night) as the illness progresses and may be so severe that they cause vomiting, broken ribs, burst capillaries, and exhaustion.
In infants, symptoms of whooping cough may be quite different and include episodes of apnea—the temporary cessation of breathing—instead of a cough.
While whooping cough is a serious and sometimes life-threatening illness that affects people of all ages, it’s especially serious in infants, who don’t receive their first pertussis vaccination until they’re 2 months old. In fact, about half of infants less than 1 year old who get pertussis need hospital treatment.
Diagnosing and Treating Whooping Cough
Because early treatment of whooping cough is important for decreasing the severity of the illness, your health care provider will speak with you about your symptoms and medical history and perform a physical exam.
As mentioned, whooping cough in the early stages resembles the common cold, so your doctor may not suspect pertussis, but a throat culture to check for the presence of Bordetella pertussis bacteria can help confirm the diagnosis.
Once a diagnosis has been established, your physician will usually elect to treat the infection with antibiotics to both decrease the severity of the infection and prevent its spread to others. However, antibiotics are generally ineffective in people who’ve been sick for at least 3 weeks, as the body has already eliminated the bacteria even though the damage they caused remains.
And, unfortunately, beyond drinking plenty of fluids and using a cool mist humidifier to help loosen mucus and soothe the respiratory tract, not much else can be done to relieve the cough. In fact, over-the-counter cough medicines have little effect on whooping cough and are discouraged.
Recovery from pertussis can be a slow process in which coughing fits begin to decrease in both severity and frequency. However, the paroxysms of coughing can still come back if the person contracts another respiratory infection in the weeks or months after a pertussis infection.
Complications of Whooping Cough
Teens and adults who contract whooping cough generally recover without any issues. If problems do develop, they tend to be side effects of the cough and include:
- Broken ribs
- Abdominal hernias
- Broken blood vessels in the skin or eyes
By contrast, infants, especially those under the age of 6 months, are at greatest risk of complications from whooping cough. These complications include:
- Encephalopathy (brain damage)
- Pneumonia
- Apnea
- Dehydration
- Weight loss
- Seizures
According to the CDC, 1 out of 4 infants with pertussis will develop pneumonia, and 1 or 2 out of every 100 will die, which is why it’s important for people who come in contact with infants to be up to date on the pertussis vaccine.
Rising Number of Whooping Cough Cases
After a vaccine became widely available in the 1940s, cases of whooping cough in the United States began to steadily decline, hitting their lowest rates in the 1970s and early 1980s. But cases then began to increase again, peaking in 2012 at 48,277—the highest number since 1955, when public health experts reported 62,786 cases.
While cases have since decreased to the high teens, this is still significantly higher than the low of 1,010 achieved in 1976. This has led public health experts to investigate the reasons underlying the recent uptick in cases. And here’s what they’ve found:
- Waning immunity: The number one reason behind the surge in cases of whooping cough appears to be diminishing levels of immunity provided by the newer acellular pertussis vaccines. While these vaccines are safer than their predecessors, the amount of protection they provide isn’t as robust. For example, one recent study found that the whooping cough vaccine is over 80% effective during the first 3 years after vaccination, but the level of protection drops to less than 50% by the eighth year. This is why keeping your immune system strong with nutritional aids such as essential amino acids is critical.
- Incomplete vaccine coverage: Some have blamed increased rates of whooping cough on the so-called anti-vaxxers—people who believe there’s a connection between vaccinations and certain health problems, especially autism. However, many experts now believe the real problem lies in the fact that adults are unaware they need boosters to make up for the lower levels of protection provided by acellular pertussis vaccines.
- Population turnover: The normal rate of people moving into and out of an area in relation to population size is also thought to play a role in the increases in cases of whooping cough.
Vaccinating for Whooping Cough
To help prevent whooping cough, the CDC recommends vaccination with diphtheria, tetanus, and pertussis (DTaP) for infants and young children and tetanus, diphtheria, and pertussis (Tdap) for preteens, teens, and adults.
DTaP is a five-shot vaccine series that protects against diphtheria, tetanus, and pertussis. It’s administered beginning at 2 months of age, with the final dose given between 4 and 6 years of age. Tdap is a booster vaccine that’s now being recommended to augment the waning immunity of acellular pertussis vaccines.
Tdap is recommended especially for adults who are in close contact with children—such as childcare workers—and pregnant women. In fact, the CDC recommends that all pregnant women receive a booster during the third trimester of every pregnancy to help provide their infants with some protection against whooping cough.
While no vaccine is 100% effective, the spread of infectious diseases like whooping cough can be reduced with an appropriate vaccination schedule. And people who are vaccinated but still get sick tend to experience milder and briefer symptoms. So if you need to update your status, don’t hesitate to contact your health care provider about getting vaccinated. Not only will you help protect yourself from this nasty bug, but you’ll help protect others too.

Up to 25% off Amino
Shop NowTAGS: conditions
Join the Community
Comments (0)
Most Craveable Recipes




 833-264-6620
833-264-6620



















